| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 9, September 2013, pages 627-632
Hypercalcemia and Peripheral T-Cell Lymphoma-Type Lymphoproliferative Disorder Associated With Methotrexate in a Rheumatoid Arthritis Patient
Jun Suzukia, b, Hitoshi Sugawarab, e, Akira Ishiib, Mitsuru Makib, Hidenori Sanayamab, Hiroshi Matsubayashib, Tamami Watanabeb, Wilfred Y. Fujimotoc, Masafumi Kakeib, Shigeki Yamadad
aDivision of Internal Medicine, Sendai City Hospital, Sendai, Japan
bDivision of General Medicine, First Department of Comprehensive Medicine, Saitama Medical Center, Jichi Medical University, Saitama, Japan
cDivision of Metabolism, Endocrinology and Nutrition, University of Washington School of Medicine, Seattle, United States
dDepartment of Pathology, Saitama Medical Center, Jichi Medical University, Saitama, Japan
eCorresponding author: Hitoshi Sugawara, Division of General Medicine, First Department of Comprehensive Medicine, Saitama Medical Center, Jichi Medical University, 1-847, Amanuma-cho, Omiya-ku, Saitama-city, Saitama 330-8503, Japan
Manuscript accepted for publication August 5, 2013
Short title: MTX-Associated Lymphoproliferative Disorder With Hypercalcemia
doi: https://doi.org/10.4021/jmc1432w
| Abstract | ▴Top |
We report the case of a 68-year-old Japanese man with rheumatoid arthritis who had progressive fatigue associated with hypercalcemia complicated by peripheral T-cell lymphoma (PTCL)-type methotrexate-associated lymphoproliferative disorder (MTX-LPD). Epstein-Barr virus (EBV) studies indicated presence of the virus in peripheral blood; however, axillary lymph-node biopsy specimen was negative. After the discontinuation of MTX, the Disease Activity Score 28-C-Reactive Protein (DAS28-CRP) improved from 2.9 to 2.2 and both hypercalcemia and lymphadenopathy remitted. We presume that both EBV reactivation under immunosuppressive state and PTCL-type MTX-LPD developing coincidentally may have contributed to hypercalcemia and consequent fatigue.
Keywords: Rheumatoid arthritis (RA); Hypercalcemia; Methotrexate (MTX); Methotrexate-associated lymphoproliferative disorder (MTX-LPD); Peripheral T-cell lymphoma (PTCL); Epstein-Barr virus (EBV); Fatigue
| Introduction | ▴Top |
Fatigue is a common symptom in primary care practice. But a definite etiological diagnosis is occasionally difficult [1]. Hypercalcemia is one of causes of fatigue, and is reported to be associated with various causes, some of which are rare [2].
Svensson et al [3] firstly showed a case of hypercalcemia and lymphoproliferative disorders (LPD) developing in a rheumatoid arthritis (RA) patient treated with methotrexate (MTX). But the specific mechanism of hypercalcemia was not shown in this setting.
MTX is a dehydrofolate reductase inhibitor and is a key drug for RA [4], and was the first reported immunosuppressive agent associated with LPD [5]. One factor that provokes MTX-LPD may be Epstein-Barr virus (EBV) infection [6].
LPD is a very important complication of MTX treatment in RA patients about which physicians should be aware. We report the case of a 68-year-old man with RA under MTX treatment developing fatigue, who had MTX-LPD resembling peripheral T-cell lymphoma (PTCL) with hypercalcemia which remitted after stopping MTX.
| Case Report | ▴Top |
A 68-year-old Japanese male had been diagnosed with RA at 56-year-old and prescribed prednisolone (PSL) (2.5 mg/day) and MTX (7.5 mg weekly) for 4 years. He had a history of well controlled hypertension and hyperuricemia during 7 years. Though he did not feel swelling nor painful joints and his RA had been controlled well two months before admission, he was seen in a local clinic because of advancing fatigue and poor appetite. He was diagnosed with depression and prescribed antidepressants. However, his poor appetite and fatigue progressed and he became too weak to walk by himself. When his local doctor found both high CRP and anemia, he was referred to our medical center for diagnosis and treatment. In addition to PSL and MTX, his medication list included folic acid, allopurinol, imidapril, bisoprolol, felodipine, trazodone, mirtazapine, and sulpiride. He reported weight loss of 14 kg during the previous two months.
His general appearance was of exhaustion and he spoke in a weak voice. Japan coma scale (JCS) was I-1. On physical examination, body temperature was 34.8 °C, blood pressure was 85/45 mmHg, heart rate was 87 beats/min and regular, and respiratory rate was 24 breaths/min. Other physical findings were pale conjunctiva, dry oral cavity, systolic murmur, hepatosplenomegaly, matted enlarged lymph nodes in the left axilla without tenderness or heat, and absent deep tendon reflexes.
Laboratory tests (Table 1) showed elevated white blood cell count, normocytic anemia, hypoalbuminemia, elevated ESR, hepatic enzymes, CRP, and serum creatinine, hypercalcemia, suppressed intact parathyroid hormone (iPTH), negative parathyroid hormone-related peptide (PTHrP) and normal 1, 25-dihydroxyvitamin D3 (1, 25-D3). The Disease Activity Score 28-C-Reactive Protein (DAS28-CRP) was 2.9 indicating moderate disease activity of RA [7].
 Click to view | Table 1. Summary of the Investigations Performed, all Positive and Relevant Negative Results are Shown |
Contrast-enhanced chest and abdominal computed tomography (CT) demonstrated enlarged left axillary lymph nodes, maximum size 6 cm by 8.5 cm (Fig. 1a), and multiple low-contrast nodules in the enlarged spleen (Fig. 1b). There were no abnormal accumulations in the 99mTc-MDP-bone scintigram.
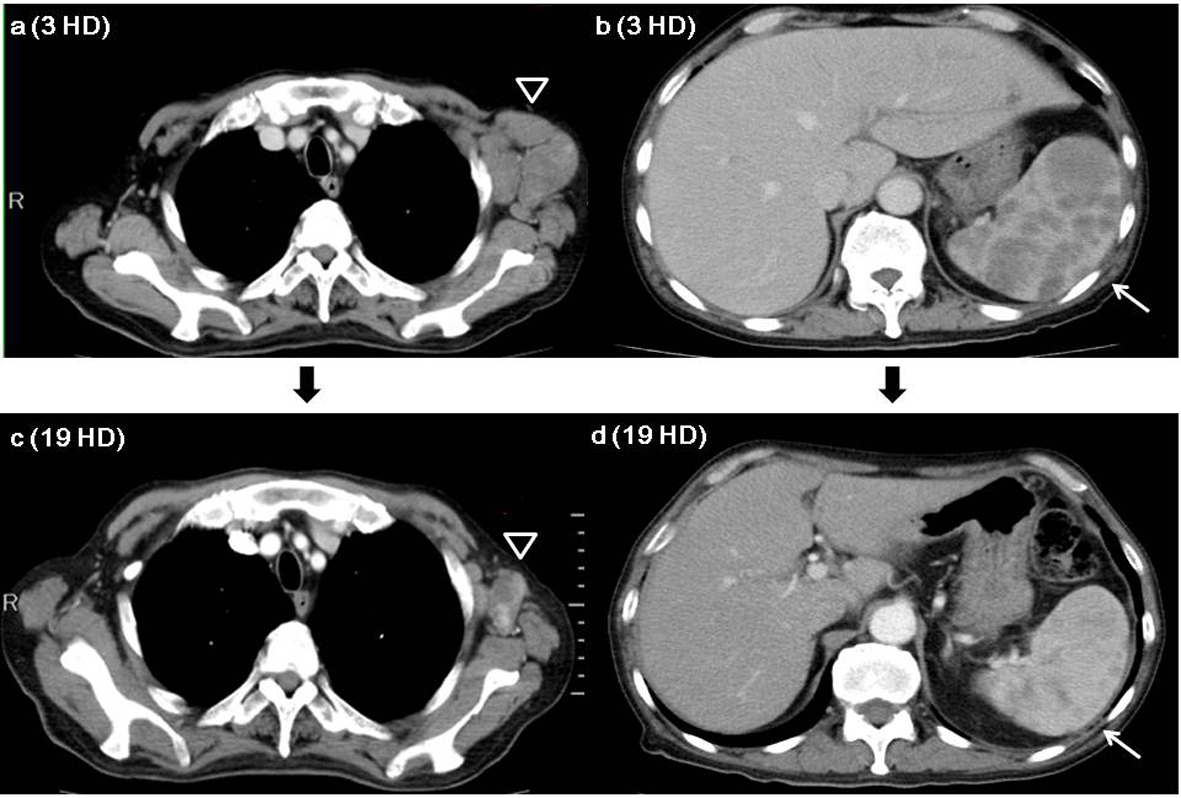 Click for large image | Figure 1. Enhanced chest and abdominal CT series. a). Chest CT on 3 HD showing enlarged left axillary lymph nodes (open triangle). b). Abdominal CT on 3 HD showing multiple low-contrast nodules in the enlarged spleen (arrow). c). Chest CT on 19 HD showing left axillary lymph nodes (open triangle) were smaller compared to the findings of chest CT on 3 HD. d). Abdominal CT on 19 HD showing low-contrast nodules have disappeared from the spleen (arrow). Abbreviations: HD; hospital day. |
Fine needle aspiration cytology from an enlarged left axillary lymph node showed large atypical cells with big nuclear bodies (Class V) (Fig. 2). CT-assisted fine needle biopsy of the lymph node showed peripheral T-cell lymphoma (PTCL) (Fig. 3a-d) including cells that were diffusely positive for T-cell markers (CD3 (Fig. 3b) and CD5) and a few cells that were weakly positive for B-cell markers (CD20 (Fig. 3c), CD79a and paired box protein 5 (PAX5)) immunohistochemically and negative for EBV-encoded RNA (EBER-1) by in situ hybridization staining (Fig. 3d). These pathological and clinical features suggested PTCL-type MTX-LPD.
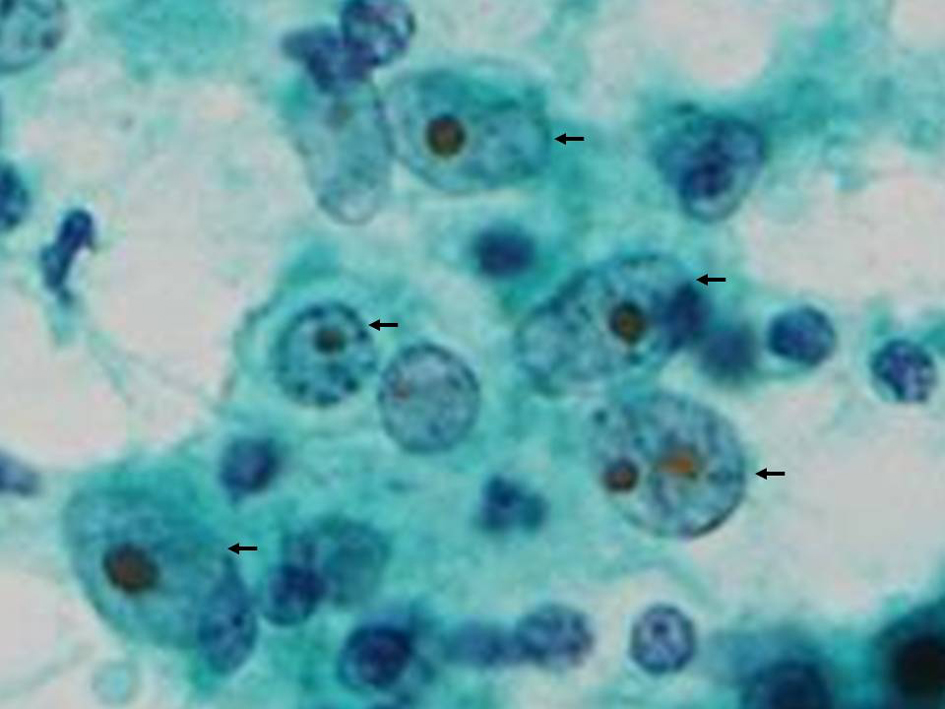 Click for large image | Figure 2. Aspiration cytology of left axillary lymph nodes. Aspiration cytology showing large atypical cells (arrows) with big nuclear body indicative class V. Original magnification, × 400, Papanicolaou stain. |
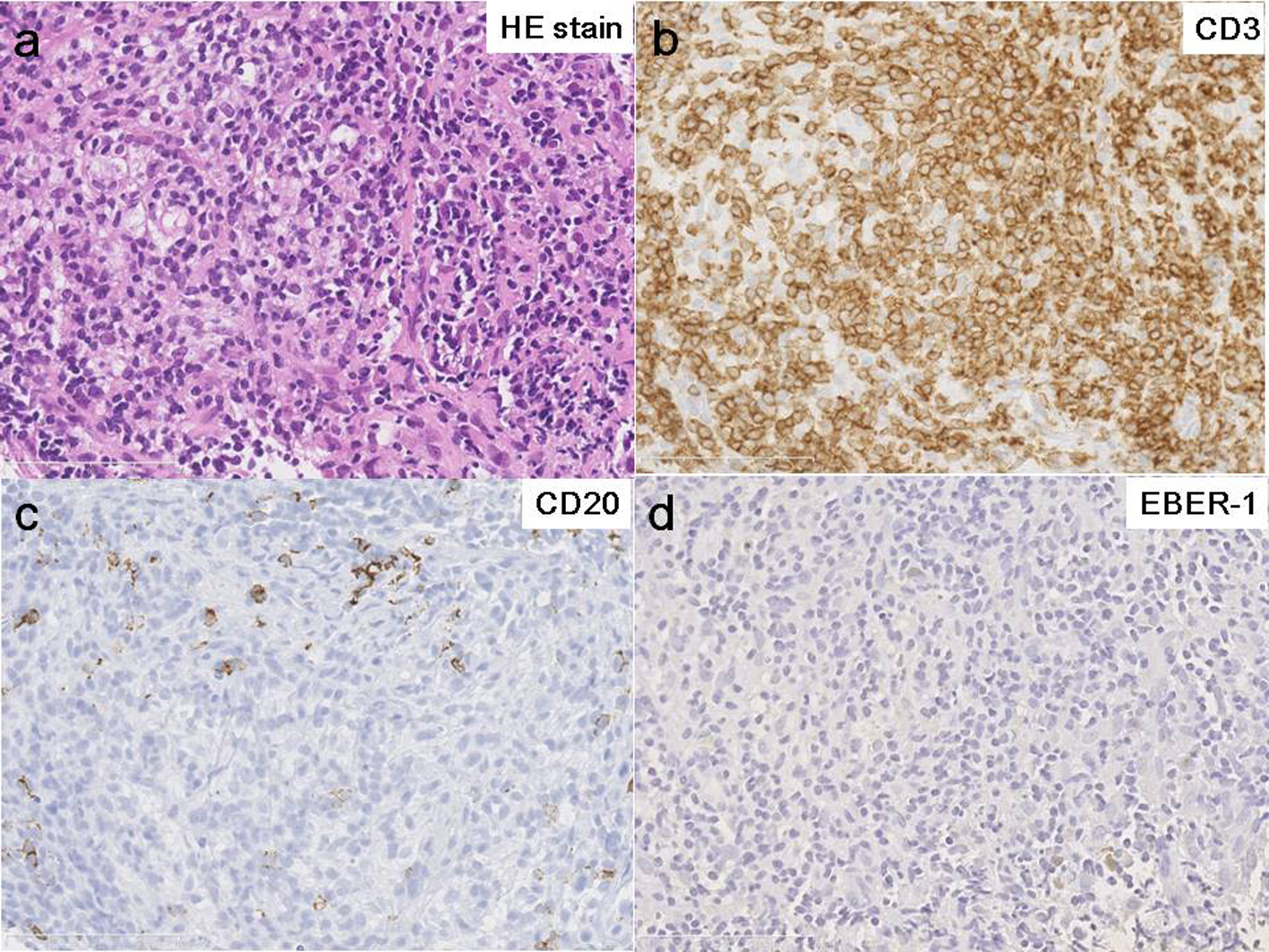 Click for large image | Figure 3. Pathology of axillary lymph nodes. Histology of biopsy specimens (HE staining) showing angioimmunoblastic lymphadenopathy-type lymphoproliferative disorder (a) including cells that were diffusely positive for T-cell marker (CD3) (b), and a few cells that were weakly positive for B-cell marker (CD20) (c) immunohistochemically and negative for EBV-encoded RNA (EBER-1) by in situ hybridization staining (d). These pathological features mimic peripheral T-cell lymphoma. Original magnification, × 400. |
MTX was stopped after admission, and daily 2.5 mg prednisolone was continued for RA treatment. Because hypercalcemia might have caused his poor appetite and fatigue, we treated with zoledronic acid and sufficient saline hydration. His fatigue gradually disappeared, his consciousness become clear, his appetite improved from hospital day (HD) 4, and he could walk by himself on HD 9. The left axillary lymphadenopathy gradually got smaller with each passing day. Serum calcium level was normalized on HD 11.
On HD 19, contrast-enhanced CT showed maximum lymph node size was 2.9 cm by 4.2 cm (Fig. 1c), intra-splenic multiple low-contrast nodules were decreased, and splenomegaly was smaller (Fig. 1d). Chemotherapy was never given during hospitalization.
The peripheral blood EBV-DNA titer was 1.4 × 103 copies/106 cells, anti-EBV associated nuclear antigen (EBNA) immunoglobulin G (IgG) was 10 times positive, and anti-EBV viral capsid antigen (VCA) IgG was 1,280 times positive on HD 22. He was discharged on HD 22 and was followed at the outpatient department in our medical center.
On day 72 after discharge (AD), the peripheral blood EBV-DNA titer was reduced to 1.1 × 102 copies/106 cells and EBV-EBNA IgG was increased from 10 times to 40 times. His joints were neither swollen nor painful and his DAS28-CRP had decreased to 2.2 consistent with reduced activity of RA.
Lymphadenopathy has not recurred during twelve months of observation. Therefore, we confirmed that he had remission of PTCL-type MTX-LPD following only cessation of MTX therapy.
| Discussion | ▴Top |
Hypercalcemia, which may be associated with both fatigue and poor appetite, was triggered by coincidental EBV reactivation during immunosuppression by MTX treatment and development of PTCL-type MTX-LPD (Fig. 4).
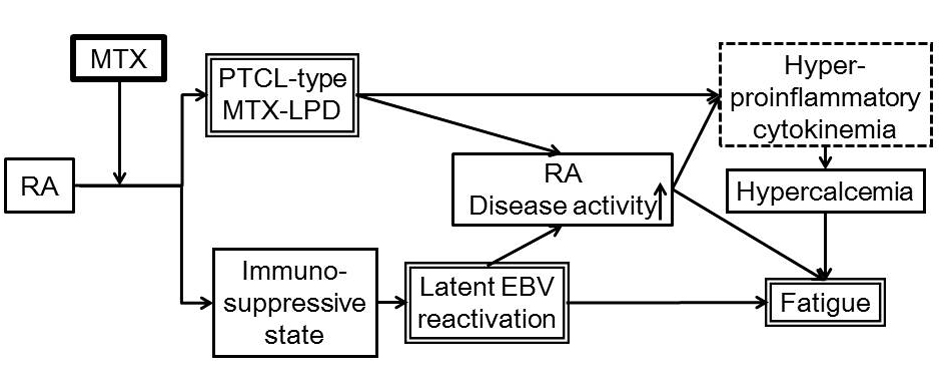 Click for large image | Figure 4. Proposed pathogenic relationship among RA, MTX-LPD, hypercalcemia and general malaise in our patient. We propose that the immuno-suppressive state induced by MTX treatment for RA reactivated latent EBV and possibly coincidentally was associated with PTCL-type MTX-LPD. Hyperproinflammatory cytokinemia resulting from both high disease activity of RA and PTCL-type MTX-LPD caused hypercalcemia and consequent fatigue. Abbreviations: RA: Rheumatoid arthritis; MTX: Methotrexate; EBV: Epstein-Barr virus; PTCL: peripheral T-cell lymphoma; MTX-LPD: Methotrexate - lymphoproliferative disease. |
Oelzner et al [8] reported that 44 of 146 patients with RA had hypercalcemia. These hypercalcemic patients had higher levels of both ESR (P < 0.01) and CRP (P < 0.05) and lower levels of both iPTH (P < 0.01) and 1, 25-D3 (P < 0.05) than those who were normocalcemic. They proposed that proinflammatory cytokines including interleukin (IL)-6 could contribute to low levels of 1, 25-D3 and iPTH in patients with high disease activity. They concluded that hypercalcemia could be associated with high disease activity of RA. These findings bear a clinical resemblance to those of our patient, though we did not have data of proinflammatory cytokines including IL-6.
The immunosuppression by MTX resulting in EBV-host imbalance [9] could cause latent EBV reactivation which induced high RA disease activity as indicated by DAS28-CRP (Fig. 4). In our patient, DAS28-CRP before and after discontinuation of MTX decreased in parallel with the numbers of peripheral EBV-DNA copies.
In our patient, PTCL-type MTX-LPD developed after four years of MTX treatment. Hoshida et al [6] reported that the rates of occurrence of MTX-LPD were 57.9% for diffuse large B cell lymphoma, 10.5% for Hodgkin lymphoma and 9.2% for PTCL. The mean duration of therapy with MTX was 54 months, with a range of 2 - 131 months when MTX-LPD developed in RA patients.
The frequency of EBV infection in MTX-LPD differed among histological types. Hoshida et al [6] reported that 27.1% of seventy six RA patients with MTX-LPD were positive for EBV. The EBV was detected in 83.3% of six Hodgkin lymphomas, 18.4% of thirty-eight diffuse large B cell lymphomas (DLBCL) and 0% of three PTCLs. EBV- DNA was detected in peripheral blood in our case, however, EBER-1 was negative in the lymph node biopsy specimen. This strongly suggests that the occurrence of reactivation of latent EBV and PTCL-type MTX-LPD may have been co-incidental.
After withdrawing MTX, numbers of EBV-DNA copies were decreased and the titer of EBV-EBNA IgG was increased. Simultaneously, both the abnormalities in the axillary lymph nodes and the spleen regressed without any chemotherapy. It has been reported that two of nine patients with MTX-LPD obtained complete remission without regrowth after withdrawal of MTX [10]. In another report [6], although eleven of forty-eight MTX-LPDs with RA obtained spontaneous regression after withdrawal MTX, five of these eleven cases showed recurrence. We must follow our patient closely for more years, although he has had no recurrence so far for twelve months.
In conclusion, fatigue might be related to hypercalcemia in our patient following increased RA disease activity. Both of PTCL-type MTX-LPD and reactivation of latent EBV infection under MTX treatment for RA were possibly related to elevation of RA disease activity. Predicting risk factors for MTX-LPD in RA patients is difficult so the possibility of this should be acknowledged by careful monitoring of the size of lymph nodes, the amount of peripheral EBV-DNA, and the level of serum calcium when MTX is given. If lymph node enlargement or hypercalcemia occurs, the first step should be to stop MTX even if the pathology may suggest malignant lymphoma.
Acknowledgments
A part of this case report was presented at the 109th Annual Meeting of the Japanese Society of Internal Medicine in Kyoto, 2012.
Grant Support
We have no grant support associated with this publication.
Conflict of Interest
All authors report no conflicts of interest associated with this publication and there has been no financial support for this paper that could have influenced its conclusion.
| References | ▴Top |
- Healey PM, Jacobson EJ. Signs and symptoms: Fatigue. in: Common medical diagnosis: an algorithmic approach 4th ed. Saunders Elsevier, Philadelphia, 2006: 2-3.
- Jacobs TP, Bilezikian JP. Clinical review: Rare causes of hypercalcemia. J ClinEndocrinolMetab. 2005;90(11):6316-6322.
doi pubmed - Svensson AM, Jacobson ER, Ospina D, Tindle BH. Reversible Epstein-Barr virus-negative lymphadenopathy and bone marrow involved by Hodgkin's lymphoma in a rheumatoid arthritis patient undergoing long-term treatment with low-dose methotrexate: a case report and review of the literature. Int J Hematol. 2006;83(1):47-50.
doi pubmed - Davis JM, 3rd, Matteson EL. My treatment approach to rheumatoid arthritis. Mayo Clin Proc. 2012;87(7):659-673.
doi pubmed - Kurtz SB, Johnson WJ. A four-year comparison of continuous ambulatory peritoneal dialysis and home hemodialysis: a preliminary report. Mayo Clin Proc. 1984;59(10):659-662.
doi - Hoshida Y, Xu JX, Fujita S, Nakamichi I, Ikeda J, Tomita Y, Nakatsuka S, et al. Lymphoproliferative disorders in rheumatoid arthritis: clinicopathological analysis of 76 cases in relation to methotrexate medication. J Rheumatol. 2007;34(2):322-331.
pubmed - Prevoo ML, van 't Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis.Arthritis Rheum. 1995;38(1):44-48.
doi pubmed - Oelzner P, Lehmann G, Eidner T, Franke S, Muller A, Wolf G, Hein G. Hypercalcemia in rheumatoid arthritis: relationship with disease activity and bone metabolism. Rheumatol Int. 2006;26(10):908-915.
doi pubmed - Hoshida Y, Tomita Y, Zhiming D, Yamauchi A, Nakatsuka S, Kurasono Y, Arima Y, et al. Lymphoproliferative disorders in autoimmune diseases in Japan: analysis of clinicopathological features and Epstein-Barr virus infection. Int J Cancer. 2004;108(3):443-449.
doi pubmed - Miyazaki T, Fujimaki K, Shirasugi Y, Yoshiba F, Ohsaka M, Miyazaki K, Yamazaki E, et al. Remission of lymphoma after withdrawal of methotrexate in rheumatoid arthritis: relationship with type of latent Epstein-Barr virus infection. Am J Hematol. 2007;82(12):1106-1109.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


