| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 6, June 2013, pages 429-432
Hand Monoparesis Due to Small Cortical Ischemic Stroke, Etiology, Prognosis and Medical Management: Case Report and Literature Review
Paula Ebolia, c, Asma Moheetb, Shlee Songb, Robert Ryana, Michael Alexandera
aDepartment of Neurosurgery, Cedars Sinai Medical Center Los Angeles California, USA
bDepartment of Neurology, Cedars Sinai Medical Center Los Angeles California, USA
cCorresponding author: Paula Eboli, Department of Neurosurgery, Cedars Sinai Medical Center Los Angeles California, 8631 W. Third St., Suite 800E, Los Angeles, CA 90048, USA
Manuscript accepted for publication April 25, 2013
Short title: Hand Monoparesis
doi: https://doi.org/10.4021/jmc1283w
| Abstract | ▴Top |
We present the case of a 70-year-old male who presented to Cedars Sinai Emergency room with sudden onset of right hand weakness. Only a few cases of hand weakness due to a small cortical stroke have been previously reported. Brain MRI showed acute small, ischemic infarction in the left right precentral gyrus and CTA showed 75% stenosis at the origin of the left internal carotid. After discussing possible risks and benefits, he received IV rTPA and underwent subsequent carotid endarterectomy a few days later. Our paper highlights the importance of considering small cortical strokes in patients with sudden onset of hand weakness since these patients may benefit from IV administration of rTPA and early intervention to treat embolic source and prevent future ischemic events.
Keywords: Cortical stroke; Omega sign; Distal embolic strokes
| Introduction | ▴Top |
Hand weakness due to cortical cerebral infarction is a rare clinical picture and has been reported to be less than 1% of all ischemic strokes [1-3]. It was first described by Lhermitte in the early nineteen hundreds as a “pseudo peripheral palsy”, weakness of the fingers due to a central nervous system lesion [3].
Some hand weakness cases have been described as pure motor weakness predominantly in the extensors muscles while others resembled ulnar or median palsies [2, 4].
It is usually caused by ischemic cortical infarcts in the MCA territory, involving the motor hand cortex, although several cases of subcortical infarcts involving the ventroposterior thalamus and posterior limb of the internal capsule have also been reported [2, 4].
| Case Report | ▴Top |
History and presentation
Patient is a right-handed 70-year-old male who was writing notes when he had sudden onset of right hand weakness. He was emergently brought to Cedars Sinai Emergency room. Upon admission he had significant right hand weakness but no difficulty with movement in the right proximal arm, no numbness and no problems with weakness in the right leg or right face. He did not have any symptoms on the left side nor changes in his speech or hearing.
He used to take daily aspirin but he had discontinued it for a couple of weeks due to planned lens surgery. He took no other medications and denied any history of TIAs or strokes in the past and had no history of cardiovascular disease.
Physical exam
Intact except for, 0/5 interosseous strength in the right hand, wrist extension was brief and not against gravity and abducens pollicis brevis strength was 2/5. Otherwise strength in the biceps, triceps and deltoid was 5/5.
Imaging
Noncontrast head CT showed no acute intracranial pathology. CTA head and neck showed 75% stenosis at the origin of the left internal carotid artery due to a mixture of calcified and noncalcified atherosclerotic disease extending from the carotid bulb (Fig. 1). No hemodynamically significant stenosis within the right internal carotid artery and no hemodynamically significant stenosis or acute vascular occlusion was identified within the proximal anterior cerebral, middle cerebral, or posterior cerebral arteries. Brain MRI showed acute small, positive on diffusion-weighted imaging, ischemic infarction in the left precentral gyrus in the location of the “Omega sign” area which innervates the right hand (Fig. 2).
 Click for large image | Figure 1. CTA head and neck showed 75% stenosis at the origin of the left internal carotid artery due to a mixture of calcified and noncalcified atherosclerotic disease extending from the carotid bulb. |
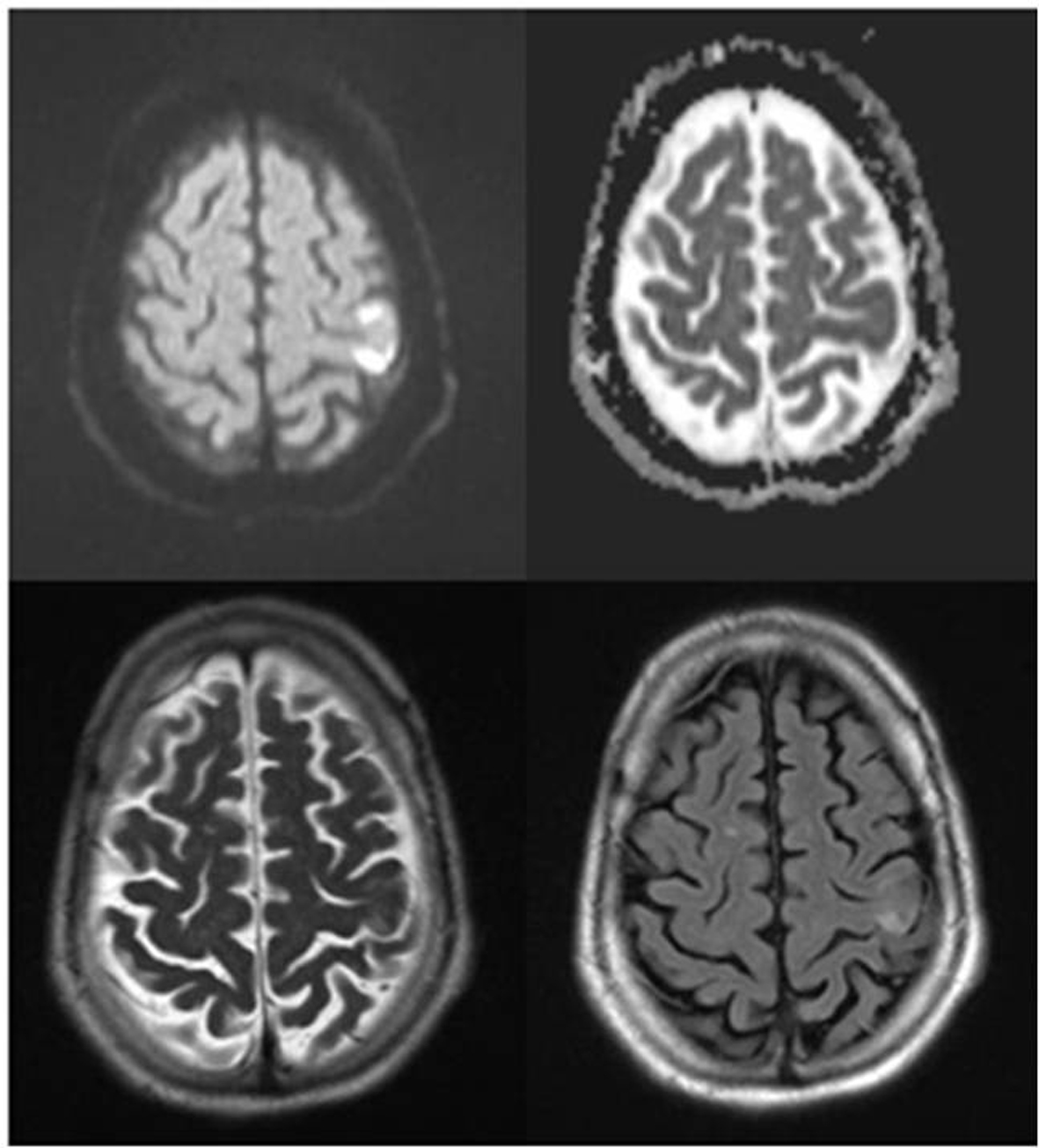 Click for large image | Figure 2. Brain MRI showed acute small, positive on diffusion-weighted imaging, ischemic infarction in the left precentral gyrus in the location of the “Omega sign” area which innervates the right hand. |
Hospital course
Although the patient’s NIH stroke scale score was 0, since his tone in his right dominant hand was flaccid and he was significantly disabled by his presenting symptoms, after discussing risks and benefits, he received IV rTPA. Patient was admitted to the neuro ICU and had some improvement of his R hand function within 24 h of TPA administration and continued to improve during his hospitalization .He was subsequently started on aspirin antiplatelet therapy and statin (Lipitor) in setting of hyperlipidemia and underwent carotid endarterectomy 3 days after his initial stroke. Post operatively he did fine and was discharged home on post op day 1with minimal residual R hand weakness.
| Discussion | ▴Top |
The cortical “hand knob” in the precentral girus has been referred to be the site of hand motor function [5]. It has been described as having an epsilon or omega shape in axial MRI or CT images [6]. In 2007 Caulo et al added 3 morphologic variants to the 2 already known and called them laterally asymmetric epsilon, medially asymmetric epsilon, and nul [6].
Strokes in this area have been widely suggested to be embolic in origin and hypertension and atherosclerosis disease have been described as the most frequently associated comorbidies [4, 5]. Many authors agree these are small cortical lesions caused by distal embolism with usually no additional tissue at risk and benign clinical course [4, 5, 7]. Despite this, etiology still remains controversial.
Peters et al reviewed 29 patients with hand area cortical strokes. Nearly all the patients had atherosclerotic changes in the carotid artery, suggesting a possible arterio-arterial embolic mechanism. They based this suggestion on previous observations that arterial embolic strokes are associated with smaller and more superficial infarcts when compared to cardiogenic ones, assuming that smaller particle size originated from an arterial source, result in more distal infarctions compared to cardiogenic embolism [5, 8].
In 2001 Gass et al studied 14 consecutive patients with acute distal arm paresis due to a cortical infarct involving the primary motor hand cortex area and concluded that these ischemic strokes are usually caused by distal embolic MCA artery occlusion, either, cardiac or arterial (artery to artery) in origin [4].
On the other hand Pikula et al recently published their 7 patients’ series with isolated arm weakness and concluded that these cases appear to have a heterogeneous etiology and found no specific pattern [2].
Many times these lesions are misdiagnosed and symptoms are assigned to lower motor neuron disease [3]. This often leads to mismanagement and incorrect workup.
According to the Guidelines for the early management of adults with ischemic stroke, both CT and MRI are being used as initial imaging diagnostic options [9]. In these cases brain MRI should be considered, if it can be easily obtained, since such a small lesion can be easily missed in CT [10].
Administration of Intravenous recombinant tissue plasminogen activator remains the most beneficial treatment for acute ischemic strokes [9]. Based on the fact that hand weakness is a measurable neurological deficit and can be very disabling, if symptoms are not spontaneously improving and patient has no contraindications, our recommendation is to proceed with IV rTPA administration; followed by a complete stroke workup and treatment of thromboembolic source and risk factors.
Conclusion
Early recognition of a small cortical stroke in patients with sudden onset of hand weakness can lead to appropriate stroke management, administration of IV TPA and early intervention if indicated to prevent further ischemic events.
Financial Disclosure Statement
We have no financial disclosures.
| References | ▴Top |
- Celebisoy M, Ozdemirkiran T, Tokucoglu F, Kaplangi DN, Arici S. Isolated hand palsy due to cortical infarction: localization of the motor hand area. Neurologist. 2007;13(6):376-379.
doi pubmed - Pikula A, Stefanidou M, Romero JR, Kase CS. Pure motor upper limb weakness and infarction in the precentralgyrus: mechanisms of stroke. J VascInterv Neurol. 2011;4(1):10-13.
pubmed - Rankin EM, Rayessa R, Keir SL. Pseudoperipheral palsy due to cortical infarction. Age Ageing. 2009;38(5):623-624.
doi pubmed - Gass A, Szabo K, Behrens S, Rossmanith C, Hennerici M. A diffusion-weighted MRI study of acute ischemic distal arm paresis. Neurology. 2001;57(9):1589-1594.
doi pubmed - Peters N, Muller-Schunk S, Freilinger T, During M, Pfefferkorn T, Dichgans M. Ischemic stroke of the cortical "hand knob" area: stroke mechanisms and prognosis. J Neurol. 2009;256(7):1146-1151.
doi pubmed - Caulo M, Briganti C, Mattei PA, Perfetti B, Ferretti A, Romani GL, Tartaro A, et al. New morphologic variants of the hand motor cortex as seen with MR imaging in a large study population. AJNR Am J Neuroradiol. 2007;28(8):1480-1485.
doi pubmed - Maeder-Ingvar M, van Melle G, Bogousslavsky J. Pure monoparesis: a particular stroke subgroup? Arch Neurol. 2005;62(8):1221-1224.
doi pubmed - Timsit SG, Sacco RL, Mohr JP, Foulkes MA, Tatemichi TK, Wolf PA, Price TR, et al. Brain infarction severity differs according to cardiac or arterial embolic source. Neurology. 1993;43(4):728-733.
doi pubmed - Adams HP, Jr., del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38(5):1655-1711.
doi pubmed - Tei H. Monoparesis of the right hand following a localised infarct in the left “precentral knob”. Neuroradiology. 1999;41(4):269-270.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


