| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 3, June 2012, pages 207-210
Clostridium Perfringens Sepsis With Massive Intravascular Haemolysis: A Rare Presentation
Carolina Paulinoa, c, Joana Silvestrea, b, Joao Goncalves Pereiraa, b, Camila Tapadinhasa, Vitor Mendesa, Pedro Povoaa, b
aPolyvalent Intensive Care Unit, Sao Francisco Xavier Hospital, CHLO, Lisbon, Portugal
bCEDOC, Faculty of Medical Sciences, New University of Lisbon, Lisbon, Portugal
cCorresponding author: Carolina Paulino, Unidade de Cuidados Intensivos Polivalente, Hospital de Sao Francisco Xavier; Centro Hospitalar de Lisboa Ocidental, Estrada do Forte do Alto do Duque; 1449-005 Lisboa, Portugal
Manuscript accepted for publication February 23, 2012
Short title: Clostridium Perfringens Sepsis
doi: https://doi.org/10.4021/jmc583w
| Abstract | ▴Top |
Massive intravascular haemolysis is a rare but well-known complication of Clostridium perfringens sepsis. Presence of fever, intravascular haemolysis, numerous spherocytes in peripheral blood smear and septic shock should raise this clinical suspicion. We describe the case of a 66-year-old male who was admitted in the Emergency Room complaining of abdominal pain, vomiting, fever and dark red urine. No relevant findings in physical examination were found. Laboratory tests revealed massive intravascular haemolysis (minimum haemoglobin of 4 g/dL). Ultrasound of the upper abdomen did not show relevant findings. Six hrs later his clinical condition suddenly deteriorated, evolving to septic shock. He was promptly admitted in the Intensive Care Unit but his condition continued to deteriorate very rapidly, with severe multiple organ failure. He died a few hrs later despite full organ support and large spectrum antibiotic therapy. Clostridium perfringens was identified in blood cultures taken before death. The post-mortem evaluation revealed a high stage of body decomposition suggesting presence of gas-producing bacteria precluding the execution of the autopsy. Though this is a very rare clinical condition, the suspicion of clostridium sepsis mandates the immediate prescription of antibiotic therapy and aggressive focus control in order to change the dismal prognosis associated with this entity.
Keywords: Clostridium perfringens; Sepsis; Intravascular haemolysis
| Introduction | ▴Top |
Clostridium perfringens (C. perfringens), formerly known as Clostridium welchii, is an anaerobic Gram-positive spore-forming bacillus [1]. It is amongst the most pathogenic species of Clostridium species, alongside with Clostridium botulinum, Clostridium tetani and Clostridium difficile.
C. perfringens can be found in samples of water, soil, and it is present in gastro-intestinal tract of healthy animals as well as in humans. It has also the ability to cause disease in humans and animals, with a rapid growth of bacterial inoculum with spore and toxins formation. There are five biotypes of C. perfringens, based on the type of toxin that is produced, type A, B, C, D and E [2]. The main toxin is the α-toxin, an enzyme that splits lecithin into phosphocholine and diglyceride, causing damage to red blood cell membrane, accounting for development of spherocytosis and subsequent intravascular haemolysis [3]. The clinical presentation of C. perfringens infection includes a variety of manifestations, such as gas gangrene, emphysematous cholecystitis, crepitant cellulitis, fasciitis and myositis. It is frequently associated with septic shock and intravascular haemolysis [4-5].
The diagnosis of intravascular haemolysis by C. perfringens should be suspected in the presence of acute anaemia with a raised mean cell haemoglobin concentration and a reduced mean cell volume, spherocytosis, negative indirect and direct Coombs test, haemoglobinemia and haemoglobinuria. It is also associated with Gram-positive rods on Gram stain of a peripheral blood smear and positive blood or tissue culture. A plain radiograph of the abdomen may reveal the presence of abscess or gas in tissues [1].
We report a case of a man that die with a C. perfringens sepsis with massive intravascular haemolysis, 22 hrs after the onset of symptoms.
| Case Report | ▴Top |
A 66-year-old male was admitted in the Emergency Room of our hospital with a 12 hrs history of fever, abdominal pain, vomiting and dark red urine. He had a past medical history of hypertension, type II diabetes mellitus, dyslipidemia, hyperuricemia and nephrolithiasis. He reportedly did not have travelled abroad namely to malaria endemic areas.
At admission, his core temperature was 38 °C, pulse rate was 106/minute, blood pressure was 157/67 mmHg. Physical examination was normal with the exception of moderate pain on palpation of the epigastric and right flank zone but without signs of peritoneal irritation.
In the initial hemogram (Table 1), haemoglobin concentration and platelet count were within the normal range with an elevation of white blood cell count. Biochemical screening showed elevation of total bilirrubin, direct bilirrubin, lactate dehydrogenase, serum aspartate transaminase, serum alanine transaminase, alkaline phosphatase and γ-glutamyltransferase. Urine analysis showed the presence of hemoglobinuria without haematuria.
 Click to view | Table 1. Laboratory Data |
A peripheral blood smear revealed spherocytosis and absence of schizocytes. The direct and indirect Coombs tests were negative. Plasmodium was not detected in microscopic examination of blood. Electrocardiogram and chest X-rays were normal. Abdominal ultrasound was performed and showed no relevant findings.
A few hours later the patient remained febrile (38 °C), tachycardic and became dyspneic. Arterial blood gases revealed severe metabolic (lactic) acidosis with pH 7.33; HCO3 12.2 mmol/L; PaCO2 16.4 mmHg; PaO2 51 mmHg; SaO2 90.8%, lactate 10.4 mmol/L. Antibiotic therapy was started with piperacilin/tazobactam 4.5 g ev qid.
He was promptly admitted to our ICU with the diagnosis of massive intravascular haemolysis. His condition deteriorated very rapidly, with the development of multiple organ failure.
He was intubated and invasive mechanical ventilation was started. Large doses of vasopressor agents were given and renal replacement therapy was immediately started, without any significant clinical improvement. The second chest x-ray showed diffuse bilateral pulmonary infiltrates and severe hypoxemia (PaO2/FiO2 ratio - 43.9 mmHg), compatible with Acute Respiratory Distress Syndrome. Laboratory data in the subsequent hours following ICU admission revealed very low levels of haemoglobin concentration and platelet count, low haptoglobin and a marked increase in creatinine and transaminases (Table 1).
Coagulation tests were compatible with disseminated intravascular coagulation.
Despite intensive therapy and supportive care, the patient died 22 hrs after the onset of symptoms and 10 hrs after hospital admission. The performance of an exchange transfusion was considered but the rapid and severe courses of the disease preclude its implementation.
The definitive diagnosis of C. perfringens sepsis was made after its identification in blood cultures for anaerobes, performed before death. The blood cultures for aerobes were sterile. Autopsy was not performed because of the advanced decomposition of the body, that took place in less then 24 hrs after death, which also pointed to the presence of gas-producing bacteria (Fig. 1).
 Click for large image | Figure 1. Body decomposition. Picture from the patient's leg taken 12 hrs after his death. It shows the advanced state of body decomposition with gaseous destruction of tissues and formation of haemorrhagic blisters, suggesting the presence of gas-producing bacteria. |
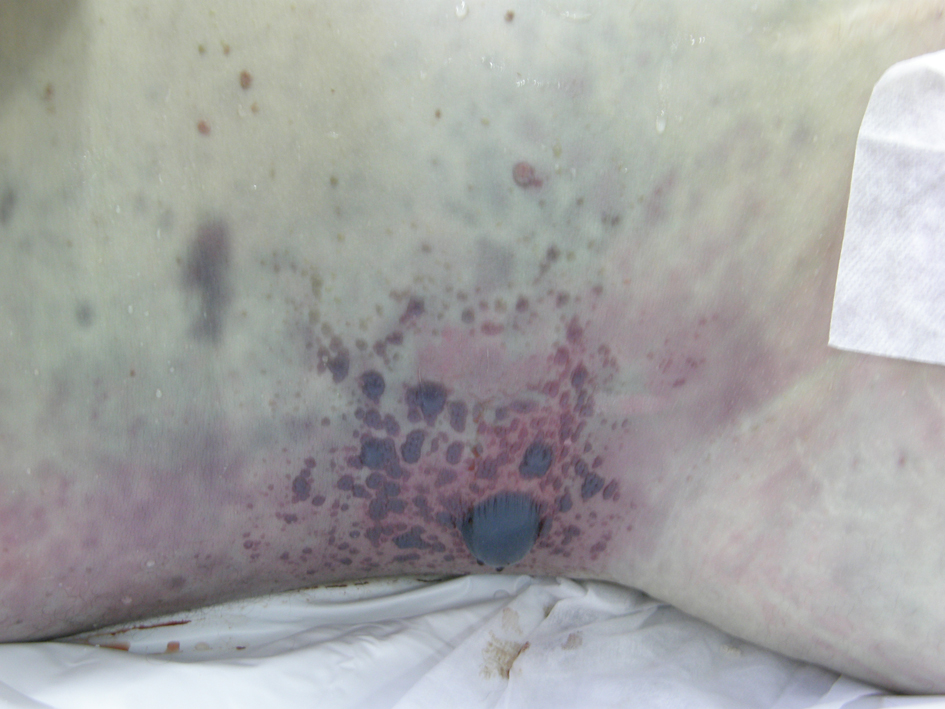 Click for large image | Figure 2. Body decomposition. Picture from the patient's right abdominal flank taken 12 hrs after his death. It shows the advanced state of body decomposition with gaseous destruction of tissues and formation of haemorrhagic blisters, suggesting the presence of gas-producing bacteria. |
| Discussion | ▴Top |
The authors present a very rare case of septic shock caused by C. perfringens bacteraemia, complicated with massive intravascular haemolysis.
Massive intravascular haemolysis is a rare but well-known complication of C. perfringens bacteraemia, occurring in 7 to 15% of cases [6], and has been considered as the most significant and unfavourable prognostic sign associated with this infection [3].
There are only a small number of diseases that cause massive intravascular haemolysis, either infectious or non-infectious. Among the infectious causes one should consider malaria, but also clostridial bacteraemia and other rare conditions, such as bartonellosis and babesiosis as possible aetiologies [7]. Nevertheless, with the exception of clostridium bacteraemia, these infectious diseases are usually straightforward to diagnose and can normally be easily excluded because of their particular epidemiology. Non-infectious causes of intravascular haemolysis include haemolytic transfusion reactions, paroxysmal nocturnal haemoglobinuria, haemolytic uremic syndrome (HUS) or haemolysis caused by snake venoms.
In our patient, the possibility of HUS was raised, since this can be associated with acute renal failure, thrombocytopenia and haemolysis. However, our patient blood smear showed spherocytes, not schizocytes typically present in this syndrome. Moreover there was no other evidence of microangiopatic haemolytic anaemia that is also characteristically present in HUS.
The diagnosis of C. perfringens sepsis is difficult without its identification in blood cultures [8]. If clostridium bacteraemia is suspected, antibiotics should be started immediately, including high-dose penicillin (up to 30 million units per day) or tetracycline (if β-lactam allergy is suspected). In the presence of gas gangrene, clindamycin is also recommended. Chloramphenicol, doxycycline, imipenem and metronidazole are also alternative agents [1]. If there is a perceived infection focus, large and rapid surgical debridement is part of the initial approach [6].
Finally two additional therapeutic options must be considered: exchange transfusion and hyperbaric oxygen therapy. Exchange transfusion could be beneficial at an early stage of intravascular haemolysis by removing toxin-damaged red cells, free haemoglobin and fibrin split products [1, 9]. The beneficial effect of hyperbaric oxygen therapy has been reported in several case series since an oxygen-rich environment promotes the death of C. perfringens and blocks the production of toxins [1].
Van Bunderen et al. reviewed 40 cases of C. perfringens septicaemia with massive intravascular haemolysis published in the literature since 1990 [6]. They found that 37.5% of patients had no underlying condition related to this infectious disease. The most common associated diseases were haematological disorders (22.5%), pancreatic or gastric cancer (12.5%). Diabetes was present in 30% of the patients, being the only risk factor in 15%. The focus of infection was mostly hepatobiliary (45.0%), being intestinal in 17.5%. A gynaecological origin, after an invasive procedure, was found in 10% of the cases [10]. The mortality rate was very high, ranging between 70 - 100% [1, 7]. In the large majority of cases the definite diagnosis was confirmed only after death [3], as it was our case.
The present case is particular and rare since it was complicated with massive intravascular haemolysis, with an extremely rapid clinical course, without identification of an obvious infectious focus, in a patient with only one predisposing factor (diabetes).
Conclusion
Despite all the medical treatments and organ support, our patient presented a very severe septic shock and had a fatal outcome.
The severity of C. perfringens infections, associated with a high mortality rate, reinforce the importance of rapid clinical diagnosis and, above all, immediate antibiotic therapy and focus control, when appropriate.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Grant Support
There were no sources of funding for this research.
| References | ▴Top |
- Rajendran G, Bothma P, Brodbeck A. Intravascular haemolysis and septicaemia due to Clostridium perfringens liver abscess. Anaesth Intensive Care. 2010;38(5):942-945.
pubmed - Morris WE, Fernandez-Miyakawa ME. [Toxins of Clostridium perfringens]. Rev Argent Microbiol. 2009;41(4):251-260.
pubmed - Ohtani S, Watanabe N, Kawata M, Harada K, Himei M, Murakami K. Massive intravascular hemolysis in a patient infected by a Clostridium perfringens. Acta Med Okayama. 2006;60(6):357-360.
pubmed - Kapoor JR, Monteiro B, Tanoue L, Siegel MD. Massive intravascular hemolysis and a rapidly fatal outcome. Chest. 2007;132(6):2016-2019.
pubmed doi - Rogstad B, Ritland S, Lunde S, Hagen AG. Clostridium perfringens septicemia with massive hemolysis. Infection. 1993;21(1):54-56.
pubmed doi - van Bunderen CC, Bomers MK, Wesdorp E, Peerbooms P, Veenstra J. Clostridium perfringens septicaemia with massive intravascular haemolysis: a case report and review of the literature. Neth J Med. 2010;68(9):343-346.
pubmed - Pun KC, Wehner JH. Abdominal pain and massive intravascular hemolysis in a 47-year-old man. Chest. 1996;110(5):1353-1355.
pubmed doi - Fujita H, Nishimura S, Kurosawa S, Akiya I, Nakamura-Uchiyama F, Ohnishi K. Clinical and epidemiological features of Clostridium perfringens bacteremia: a review of 18 cases over 8 year-period in a tertiary care center in metropolitan Tokyo area in Japan. Intern Med. 2010;49(22):2433-2437.
pubmed doi - Uppal A, Hymes K, Schwartz DR. A 61-year-old-man with massive intravascular hemolysis. Chest. 2009;136(5):1424-1427.
pubmed doi - Bryant CS, Perry L, Shah JP, Kumar S, Deppe G. Life-threatening clostridial sepsis in a postmenopausal patient with degenerating uterine leiomyoma. Case Report Med. 2010;2010:541959.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


