| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 6, Number 3, March 2015, pages 119-121
Abdominal Skin Metastases Still Mystery
Katarzyna Mecha, d, Lukasz Masiorb, Mariusz Fraczekb, Marcin Lipinskic
aDepartment of General, Oncological and Gastroenterological Surgery Medical University of Warsaw, Public Central Teaching Hospital in Warsaw, Poland
bDepartment of General and Liver Surgery Medical University of Warsaw, Public Central Teaching Hospital in Warsaw, Poland
cDepartment of Pathology Central Clinical Hospital of the Ministry of Interior and Administration, Poland
dCorresponding Author: Katarzyna Mech, Department of General, Oncological and Gastroenterological Surgery Medical University of Warsaw, Public Central Teaching Hospital in Warsaw, Poland
Manuscript accepted for publication January 29, 2015
Short title: Abdominal Skin Metastases
doi: http://dx.doi.org/10.14740/jmc2064w
| Abstract | ▴Top |
The incidence of pancreatic cancer has been on the rise. Unfortunately, in most cases this cancer is diagnosed in an advanced stage. In clinical practice, patients with metastases to distant organs such as the liver, peritoneal cavity, lungs and even bones or brain are frequently encountered. On the other hand, skin metastases are very rare. Those that occur in the umbilical area are called Sister Mary Joseph’s nodules. Below, we present a patient who, after a long diagnostic process including removal of abdominal skin tumor, was finally diagnosed with pancreatic cancer.
Keywords: Pancreatic cancer; Metastases to the skin; Sister Mary Joseph’s nodules
| Introduction | ▴Top |
Despite the progress in diagnosis and treatment, the outcome of pancreatic cancer treatment remains unsatisfactory [1]. This is due in part to relatively late manifestation of clinical symptoms. In 80-90% of patients, the disease is detected in a locally advanced stage or after cancer has already metastasized to distant places [1-3].
The most frequent distant metastases in pancreatic cancer are liver, pleural cavity, lung, bone and brain metastases [1-5]. Skin metastases are rare, and occur only in 0.3-0.7% of patients [5].
The metastases in the umbilical area are called Sister Mary Joseph’s nodules [1-3, 5, 6] and in about 50% of cases, they come from the gastrointestinal tract. The most frequent cancers of gastrointestinal tract giving coetaneous umbilical metastasis are: gastric cancer and colorectal cancer (about 40%), but it also happens in pancreatic cancer. Pancreas as the primary site of umbilical metastases accounts for 7-9%.
We present the case of the patient, in whom the appearance of the skin nodules did not lead to fast diagnosis of the pancreatic cancer. We would like to remind our colleagues taking into consideration malignant diseases coming from internal organ especially from the pancreas during diagnosing skin lesions.
| Case Report | ▴Top |
A 76-year-old patient, living alone, a smoker of many years, with a history of duodenal ulcers and spondylosis, was admitted to the Department of Internal Medicine because of abdominal pain, especially after meals, weight loss (10 kg over a period of 2 months), and multiple oozing nodules on the abdominal skin.
According to the patient, about half a year ago, a nodular mass appeared in the umbilical area. A family physician diagnosed umbilical hernia. After approximately 2 months, the patient began experiencing extensive pain, which increased after meals, and odynophagia which limited her food intake. Moreover, in addition to earlier mild pain in the lumbar spine area, pain in the thoracic spine area developed.
An abdominal ultrasound was performed on an outpatient basis and approximately 6 cm of fluid was detected in the right pleural cavity (in the posterior auxiliary line). No significant pathological abnormalities were detected in other organs.
In a physical examination, the following observations were made: reduced vesicular sounds on the right side up to the scapular angle, and normal vesicular sound on the left side. The patient had no symptoms of shortness of breath. Irregular heart beat was approximately 90/min. The abdomen was soft, with normal peristalsis, slight pain in the epigastric area, and Blumberg’s sign was negative. Numerous nodules, from several millimeters to 4 cm in size, were palpable on the abdominal skin. The skin over the nodules was erythematous, oozing. The inguinal lymph nodes were enlarged on both sides. There were numerous seborrheic varucas, and the largest one was on the left breast. No pathological abnormalities were found in the breast. No peripheral edema was observed.
No significant abnormalities were found in laboratory tests. TSH level was normal. The potassium level increased during the hospitalization but was readily corrected. Tests for cancer markers were performed and showed CA of 15.3 - 31.18 U/mL, CA of 125 - 819.70 U/mL, CEA of 131.70 ng/mL, and CA-19.9 of 9.66 U/mL.
In an upper gastrointestinal tract endoscopy, inflammatory lesions were detected in the cardia of the stomach. Thickened, infiltrated mucosal folds were found in the body and fundus of the stomach.
In a lower gastrointestinal tract endoscopy, a polyp in the sigmoid colon, sigmoid diverticulosis and hemorrhoids were observed.
A computed tomography of the abdominal cavity was performed, in which a large, abnormal tumorous mass, approximately 67 × 85 × 70 mm in size, with obliterated boundaries was detected which infiltrated the surrounding adipose tissue with the signs of infiltration of the nearby organs - the stomach, spleen, kidney and left adrenal gland. The liver showed the signs of steatosis, and focal abnormalities were visible: approximately 18 mm in segment VIII/IVa, approximately 14.8 in segment IVb, and approximately 29 mm in segment VII. Left renal artery and vein were also infiltrated by neoplasm. Numerous enlarged pathological lymph nodes were found: periaortic, in the hepatic hilum up to approximately 19 mm, mesenterial up to approximately 23 mm, and inguinal on both sides up to approximately 21 mm. Focal abnormalities were found in the dermis (two nodules), probably skin metastases. In the part of the chest which was observed in the examination, in the pulmonary parenchyma, multiple nodules with the structure characteristic of metastases were found. Fluid in the right pulmonary cavity, an up to 6 cm fluid layer at the posterior wall of the chest was found (Fig. 1, 2).
 Figure 1. Metastasis in the umbilicus area. Figure 1. Metastasis in the umbilicus area. |
 Figure 2. Tumor in pancreas. Figure 2. Tumor in pancreas. |
To definitively determine the origin of the metastases, a piece of skin, 4.5 × 3.2 cm in size, with the subcutaneous tissue was collected and sent for histopathological examination. Macroscopic picture showed on a cross-section, in the subcutaneous tissue, a cream-like, cohesive tumor, 3.6 × 2 × 1.7 cm in size, which caused skin elevation. The microscopic picture pointed to adenocarcinoma which most likely originated in the pancreas or bile ducts. This was supported by an immunohistochemical examination: CK7 (+) [6]. Taking into account the clinical picture and additional tests performed, disseminated cancer originating in the pancreas was diagnosed (Fig. 3, 4).
 Figure 3. Histomorphologic appearance of pancreatic metastasis. Figure 3. Histomorphologic appearance of pancreatic metastasis. |
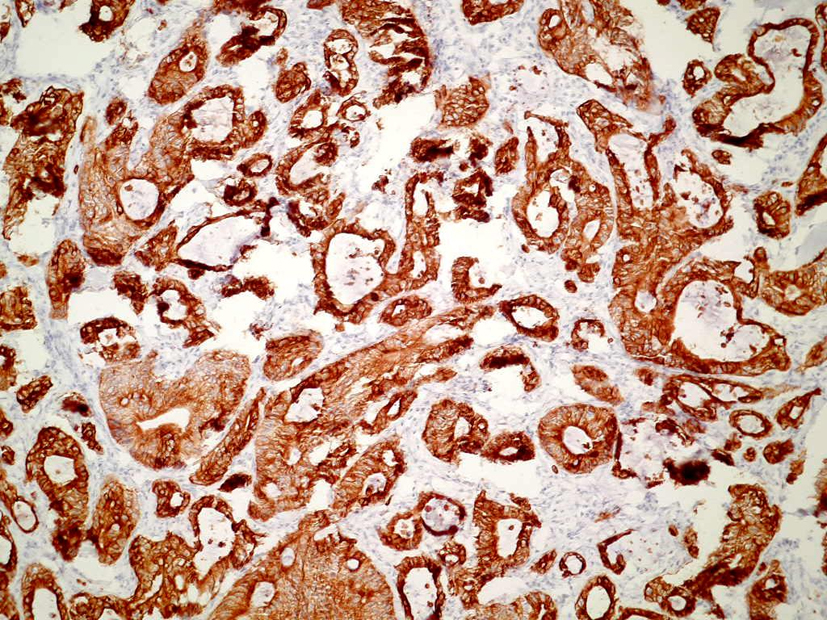 Figure 4. Immunostaining (CK7). Figure 4. Immunostaining (CK7). |
Because of the advanced stage of the disease, the patient was referred for palliative treatment.
| Discussion | ▴Top |
The mechanism of metastases development is not well understood; there are several theories which address this issue. The first one emphasizes the role of the blood circulation, the second one focuses on the lymphatic system [2], and the third one focuses on the dissemination of neoplastic cells during resection. Recently, the role of chemokines in the process of metastasis has attracted a lot of attention [1, 4, 6, 7]. According to the literature, the umbilical area is the location of the most frequent skin metastases [1, 4] but this does not mean that they do not occur elsewhere. The case of pancreatic cancer which metastasized to the skin of the neck, chest and abdomen, described by Muhammad Wasif Saif’ from the Columbia University of Physicians and Surgeons [4] in 2011 shows that each patient requires careful, individual diagnostics which is indispensable for selecting appropriate treatment.
In the case presented, the appearance of dermal nodules in the umbilicus was the reason why the patient went to see a doctor. Thus this patient is in the group of 30% of the patients in whom the appearance of skin metastases is the first sign of the disease [8]. In this case the disease was misdiagnosed by the family doctor and by patient soon after other symptoms occurred indicating malignant disease. The broader diagnostic was made and we were taking into consideration gastric cancer, colorectal cancer, breast cancer, ovarian cancer and of course pancreatic cancer. Certain irregularity in the diagnostics performed at the beginning was the result of the description of the ultrasound performed on an outpatient basis which the patient brought to the Department. Unfortunately, computed tomography also did not unequivocally confirm the presence of the tumor developing in the pancreas. This was most probably due to large dimensions of the primary lesion and infiltration of the nearby tissues. According to the literature, the development of Sister Mary Joseph’s nodules in pancreatic cancer is most often associated with the primary lesion location in the body or tail of the pancreas [1-3, 5]. Only 30% of pancreatic tumors are located in the body or tail of the pancreas and their course is associated with few symptoms. Such was the case with the patient presented and this undoubtedly contributed to the fact the correct diagnosis was made late.
Conclusions
To summarize, in differential diagnostics of the skin lesions classified as metastases, pancreatic cancer should be taken into consideration, especially if other causes, such as melanoma, lung, colon, oral, stomach cancer, and, in females ovarian and breast cancer, are eliminated [8, 9]. This occurs rarely, but as shown by numerous reports, including this one, is not impossible. Unfortunately many doctors forget in general about metastases of internal malignant diseases diagnosing skin lesions. Among other things, this is the reason why those patients are diagnosed so late and results of treatment are even more poor.
| References | ▴Top |
- Hafez H. Cutaneous pancreatic metastasis: a case report and review of literature. Indian J Cancer. 2007;44(3):111-114.
doi pubmed - Yendluri V, Centeno B, Springett GM. Pancreatic cancer presenting as a Sister Mary Joseph's nodule: case report and update of the literature. Pancreas. 2007;34(1):161-164.
doi pubmed - Pontinen T, Melin A, Varadi G, Khanmoradi K, Chewaproug D, Kung SC, Zaki R, et al. Cutaneous metastasis of pancreatic adenocarcinoma after kidney transplant: a case report and review of the literature. Exp Clin Transplant. 2010;8(4):273-276.
pubmed - Saif MW, Brennan M, Penney R, Hotchkiss S, Kaley K. Cutaneous metastasis in a patient with pancreatic cancer. JOP. 2011;12(3):306-308.
pubmed - Jun DW, Lee OY, Park CK, Choi HS, Yoon BC, Lee MH, Lee DH. Cutaneous metastases of pancreatic carcinoma as a first clinical manifestation. Korean J Intern Med. 2005;20(3):260-263.
doi pubmed - Umbilical mass as the sole presenting symptom of pancreatic cancer: a case report. Fabio Crescentini; Fernanda Deutsch; Carlos Walter Sobrado; Sergio de Araujo Rev.
- Ozaki N, Takamori H, Baba H. Sister Mary Joseph's nodule derived from pancreatic cancer. J Hepatobiliary Pancreat Sci. 2011;18(1):119-121.
doi pubmed - Colla TG, Lovatto L, Duquia RP. Case for diagnosis: umbilical metastasis of pancreatic carcinoma (Sister Mary Joseph's Nodule). An Bras Dermatol. 2009;84(3):297-298.
doi pubmed - Onkologia. Textbook for students and doctors. Radzislaw Kordek. Third edition. Via Medica. 2007.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








