| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 7, July 2016, pages 282-285
Nutcracker Phenomenon With Wilkie’s Syndrome in a Patient With Rectal Cancer
Sohail Iqbala, c, Kashif Siddiqueb, Usman Saeedb, Zahid Anwar Khanb, Sarfraz Ahmadb
aRoyal Preston Hospital, Lancashire Teaching Hospital NHS Trust, Sharoe Green Lane North, Preston, PR2 9HT, UK
bRoyal Blackburn Hospital, East Lancashire NHS Trust, Haslingden Road, Blackburn, BB2 3HH, UK
cCorresponding Author: Sohail Iqbal, Royal Preston Hospital, Lancashire Teaching Hospital NHS Trust, Sharoe Green Lane North, Preston, PR2 9HT, UK
Manuscript accepted for publication May 09, 2016
Short title: Nutcracker Phenomenon With Wilkie’s Syndrome
doi: http://dx.doi.org/10.14740/jmc2532w
| Abstract | ▴Top |
Entrapment of the left renal vein between superior mesenteric artery (SMA) and aorta can be asymptomatic or present as microscopic hematuria and orthostatic proteinuria. It can be associated with other abdominal vascular compression syndromes and duodenal obstruction. We present a 62-year-old Caucasian male patient with nutcracker phenomenon and SMA syndrome secondary to rectal cancer associated cachexia. Computed tomographic angiography is a non-invasive diagnostic modality which depicts it in great details. Its early clinical suspicion and radiologic assessment help in patient management to avert possible complications such as blood loss in already debilitating patients such as ours.
Keywords: Nutcracker phenomenon; Nutcracker syndrome; Superior mesenteric artery syndrome; Cachexia; Rectal cancer
| Introduction | ▴Top |
The replacement of normal inverted J-shaped origin of superior mesenteric artery (SMA) with acutely angulated branch off of the aorta can reduce the aortomesenteric distance, which, in turn, can compress left renal vein and the third part of duodenum between these two vessels, namely aorta and the SMA. This anatomical variant is known as nutcracker phenomenon when it is asymptomatic. In symptomatic cases, it can be termed as nutcracker syndrome or left renal vein entrapment. Sometimes, the nutcracker phenomenon, nutcracker syndrome and left renal vein entrapment are all used interchangeably [1].
| Case Report | ▴Top |
We present an interesting case of nutcracker phenomenon with an acquired SMA syndrome in a 62-year-old man, who developed significant weight loss (cachexia) due to rectal carcinoma. He underwent a contrast-enhanced CT scan as a follow-up to his rectal carcinoma. The scan revealed sloping origin of the SMA from the aorta. Aortomesenteric angle was measured to be 19° (Fig. 1) and aortomesenteric distance of 5.8 mm was calculated (Fig. 2), which confirmed the nutcracker phenomenon. There was dilatation of the lateral part and compression of the medial part of the left renal vein between the aorta and the superior mesenteric vein. The left gonadal vein was also distended, compared to its right counterpart. Moreover, the third part of the duodenum was compressed (Fig. 3a), causing proximal duodenal and gastric dilatation (Fig. 3b). The patient had non-specific symptoms which were treated conservatively and a follow-up was arranged. His previous CT in 2012 showed normal aortomesenteric arterial relationship.
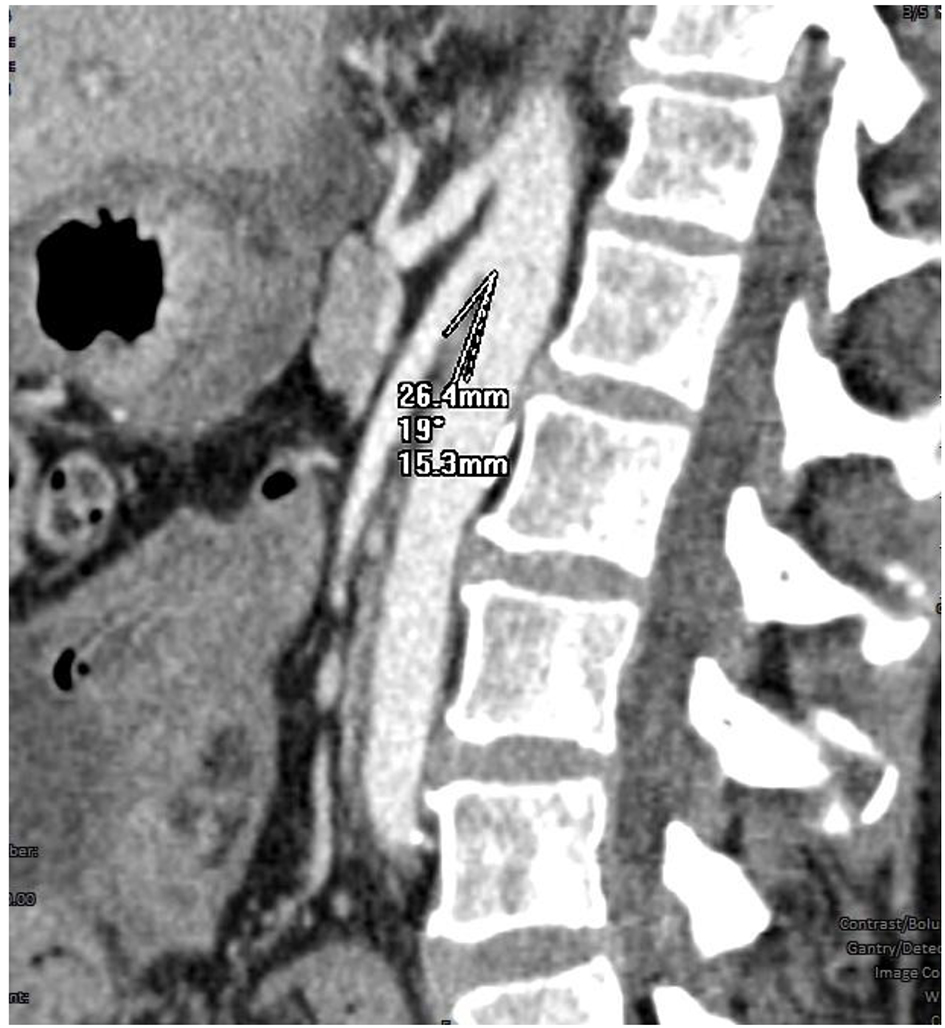 Click for large image | Figure 1. Angle between aorta and superior mesenteric artery measured to 19°. |
 Click for large image | Figure 2. Aorto-SMA distance 5.8 mm. |
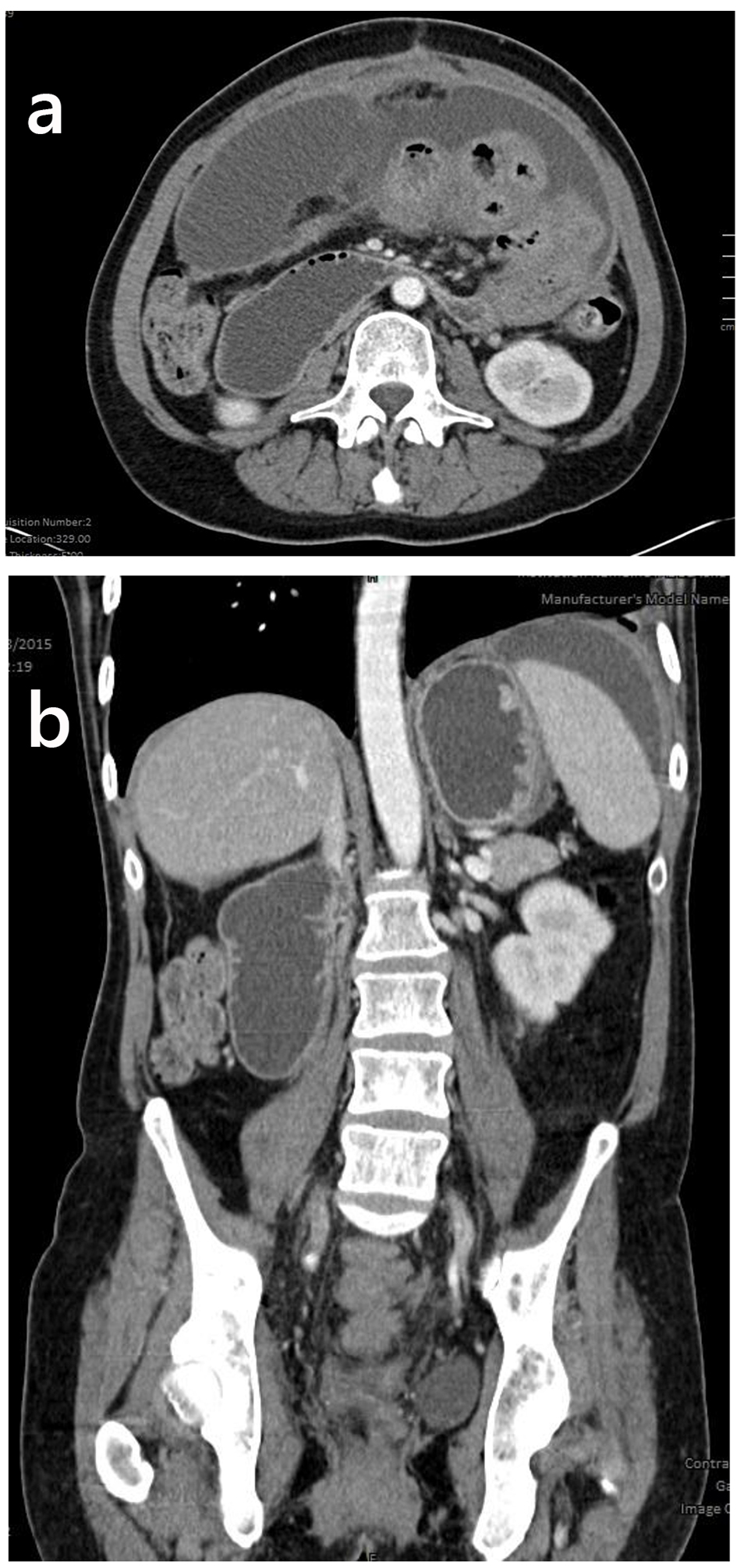 Click for large image | Figure 3. (a) Compressed third part of the duodenum. (b) Dilatation of the stomach, second part of the duodenum and partly visible renal and gonadal veins in a coronal reconstruction of the CT scan. |
| Discussion | ▴Top |
Nutcracker syndrome is a set of symptoms commonly caused by entrapment or compression of left renal vein due to nutcracker anatomy, although right-sided renal vein compression can also occur but is a rare condition. The syndrome can be divided into three types on the basis of anatomy: anterior, posterior and mixed [2]. Anterior nutcracker syndrome is characterized by compression of left renal vein between the abdominal aorta and the SMA due to acute aortomesenteric angulation and decreased aorto-SMA distance. On the other hand, posterior nutcracker syndrome results from retroaortic compression of left renal vein between the abdominal aorta and the vertebral column with a relative incidence of 17%. Mixed type accounts for 3% and has double tributaries, both anterior and posterior. The normal aortomesenteric angle is 25-90° and the normal aortomesenteric distance is 10 - 28 mm. An abnormal angle is less than 25° and an abnormal distance is 2 - 8 mm [3]. Nutcracker phenomenon can be a normal variant in the absence of clinical signs and symptoms. Rapid increase in body height and rapid weight loss are well reported causes of acquired nutcracker syndrome. The left renal vein duplication, ectopic ventral right renal artery, overarching testicular artery, abdominal aortic aneurysms, pancreatic and retroperitoneal tumors, para-aortic lymphadenopathy, left renal ptosis, lordosis, low body mass index [4] and strangulating fibrolymphatic tissue have all positive correlation with the development of nutcracker syndrome. The exact incidence is unknown. Women are more commonly affected in their third and fourth decades of life [5]. The nutcracker syndrome entails a constellation of variable symptoms, depending on the site, degree and extent of the renal vein compression. Clinically the syndrome can be divided into typical and atypical subtypes on the basis of presentation. The typical clinical presentation consists of microscopic or macroscopic unilateral hematuria and orthostatic proteinuria with or without loin pain; whereas, atypical presentation includes abdominal pain, fatigue, orthostatic intolerance, varicocele in males [6] and dysmenorrhoea in females. The English literature has demonstrated the concomitance of nutcracker syndrome with SMA syndrome. The radiological incidence of SMA syndrome in general, ranges between 0.2% and 0.78% [7]. It is three times more prevalent among females mainly in their fourth decade of life. Likewise nutcracker syndrome, SMA syndrome can be congenital or acquired. Amongst acquired causes, rapid significant weight loss is the most considerable risk factor in adults for the development of SMA syndrome. In addition, rapid increase in height without simultaneous weight gain, neurological disorders and anomalies of spine are important factors contributing to the pathology in older children and adolescents. Clinical understanding of the signs and symptoms of these two syndromes makes ground for the diagnosis. Urine analysis for hematuria and orthostatic proteinuria in the presence of clinical features is a good indicator [8]. Color Doppler ultrasound scanning can be the first baseline test in patients with clinical suspicion of nutcracker syndrome [9]. It has shown sensitivity of 78% and specificity of 100%. Ultrasound scanning coupled with Doppler can measure the length and diameter of the left renal vein, the pressure gradient between left renal vein and inferior vena cava, mean SMA-aorta angle and distance, and the flow velocity and acceleration in both supine and standing positions. However, there are certain limitations of its use in children because of smallest left renal vein sampling area and the largest Doppler angle. Cross-sectional imaging plays a vital role in the depiction of anatomical details. Computed tomography angiography (CTA) is superior to all modalities in confirming the diagnosis by delineating the aberrant anatomy; measuring the aorto-SMA angle and the distance; and the amounts of intra-abdominal and retroperitoneal fat. In addition, CT scan can manifest associated findings including gonadal vein dilatation, varicosities and duodenal dilatation. CTA and magnetic resonance angiography (MRA) are very useful in demonstrating the anatomy, providing precise details of the LRV compression, and dilatation points and of perirenal or gonadal varices. CTA has reported sensitivity of 91.7% and specificity of 88.9% [10]. Although MRA is superior to CTA and venography in being less invasive, retrograde venography is the gold standard to confirm the diagnosis of nutcracker syndrome [11]. It gives all information about the anatomy and the pressure gradient across the compression point. In addition, cystoscopy may help indirectly to make diagnosis of NCS by confirming unilateral hematuria. Conventional imaging like plain X-ray abdomen can show the presence of gas in the stomach and duodenum with paucity of distal bowel gases in case of duodenal obstruction thus, supporting the diagnosis of SMA syndrome. Likewise, Barium studies can be helpful in demonstrating the signs of duodenal obstruction. A positive Haye’s maneuver or jejunum contrast flow study is the preferred baseline diagnostic test in most of the SMA syndrome cases. In symptomatic cases, intravascular stenting is the preferred management technique. Extravascular stenting is an alternate method. In severe cases, laparoscopic re-implantation or open surgery for correction of the angle may be carried out [12]. Nephrectomy and renal transplant is reserved for extreme cases. Correction of associated conditions is also contemplated in selected cases.
Learning points
The nutcracker phenomenon can be asymptomatic with benign clinical course; however, the nutcracker syndrome can be severely symptomatic and can cause significant morbidity.
Duodenal obstruction is a hallmark of Wilkie’s syndrome which is a well-reported association of the nutcracker phenomenon.
Color Doppler and CECT are sensitive diagnostic modalities in such cases.
Conflicts of Interest
None.
Financial Disclosure
None.
| References | ▴Top |
- Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc. 2010;85(6):552-559.
doi pubmed - Mallat F, Hmida W, Othmen MB, Mosbah F. Mixed nutcracker syndrome with left renal vein duplication: A severe and exceptional presentation in an 18-year-old boy. Urol Ann. 2015;7(2):244-247.
doi pubmed - Fong JK, Poh AC, Tan AG, Taneja R. Imaging findings and clinical features of abdominal vascular compression syndromes. AJR Am J Roentgenol. 2014;203(1):29-36.
doi pubmed - Sharp G, Glenn D. A Differential Diagnosis of Haematuria following a Motor Vehicle Collision: Nutcracker Syndrome. Case Rep Surg. 2015;2015:749182.
doi - Rudloff U, Holmes RJ, Prem JT, Faust GR, Moldwin R, Siegel D. Mesoaortic compression of the left renal vein (nutcracker syndrome): case reports and review of the literature. Ann Vasc Surg. 2006;20(1):120-129.
doi pubmed - Hmida W, Mallat F, Othmen MB, Limayem F, Mosbah F. Modified medial nephropexy for treatment of the anterior nutcracker syndrome. Urol Ann. 2014;6(4):352-355.
doi pubmed - Mathenge N, Osiro S, Rodriguez, II, Salib C, Tubbs RS, Loukas M. Superior mesenteric artery syndrome and its associated gastrointestinal implications. Clin Anat. 2014;27(8):1244-1252.
doi pubmed - Jin M, Hu P, Ding R, Chen P, Qiu Q, Wu J, Liu S, et al. Effectiveness of supine/standing urinalysis for differential diagnosis of left renal vein entrapment syndrome combined with or without glomerulopathy. Nephrology (Carlton). 2014;19(6):332-338.
doi pubmed - Inal M, Unal Daphan B, Karadeniz Bilgili MY. Superior mesenteric artery syndrome accompanying with nutcracker syndrome: a case report. Iran Red Crescent Med J. 2014;16(10):e14755.
doi pubmed - Gulleroglu K, Gulleroglu B, Baskin E. Nutcracker syndrome. World J Nephrol. 2014;3(4):277-281.
doi pubmed - Yun SJ, Nam DH, Ryu JK, Kim JS. The roles of the liver and pancreas in renal nutcracker syndrome. Eur J Radiol. 2014;83(10):1765-1770.
doi pubmed - Shao P, Li P, Ju X, Qin C, Yin C. Retroperitoneal laparoscopic reimplantation of the left renal vein for nutcracker syndrome. Urol Int. 2015;94(1):74-78.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


