Figures
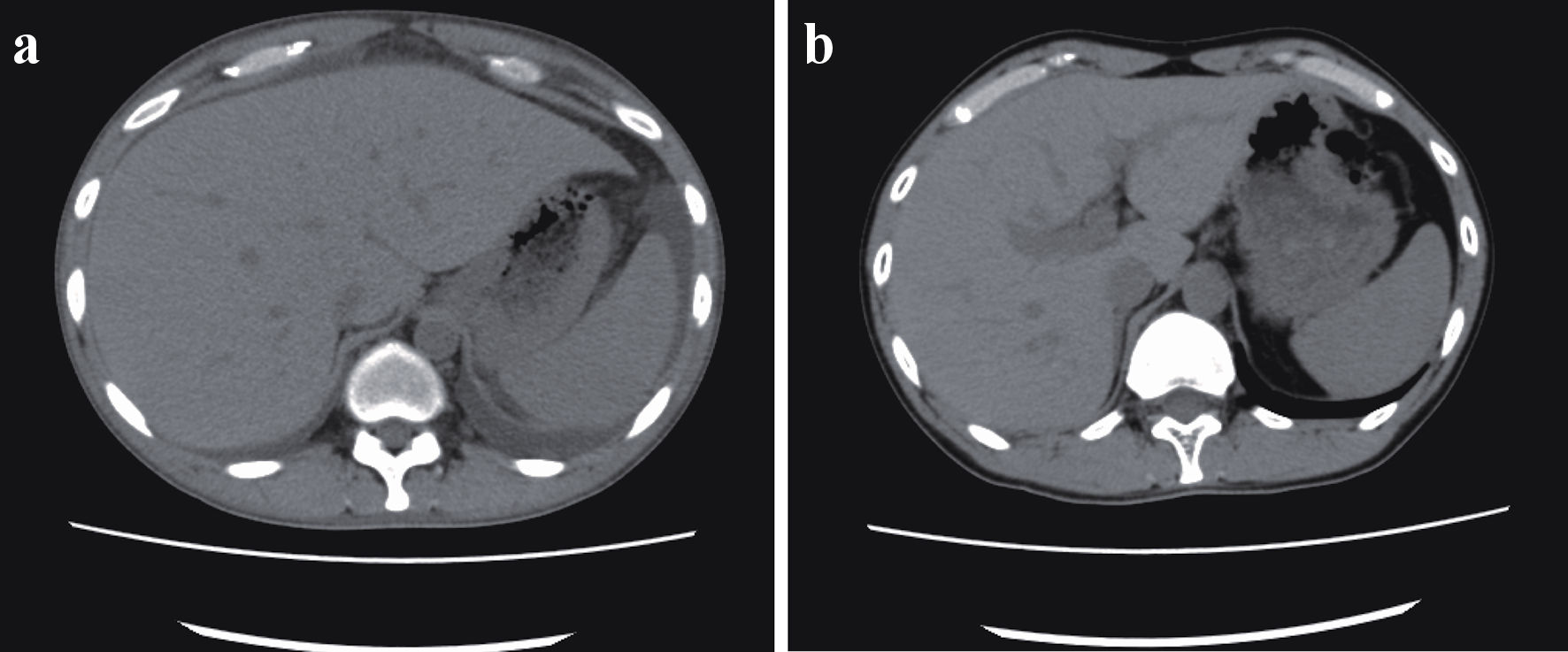
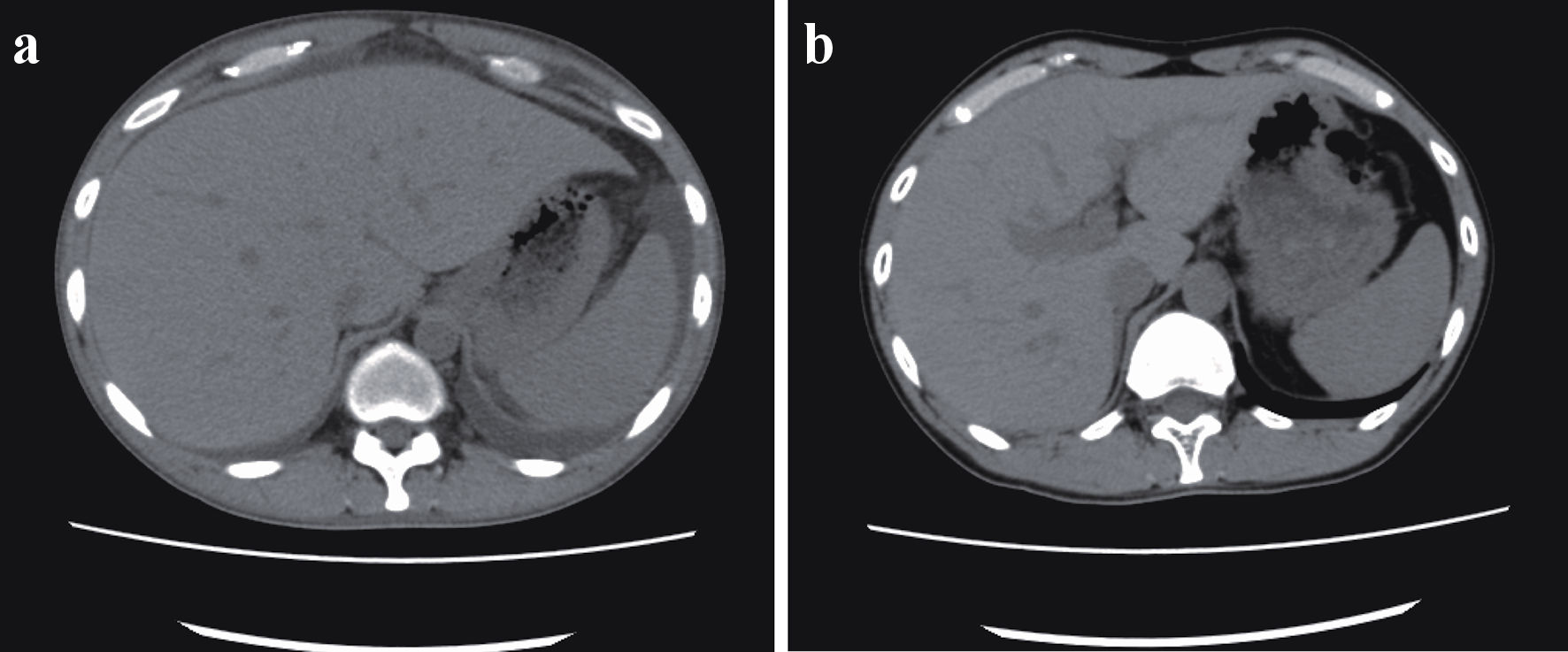
Figure 1. (a) Ascites before cyclosporine therapy. Whole-body computed tomography revealed bilateral ascites, pleural effusion, anasarca, generalized lymphadenopathy, and hepatosplenomegaly before the initiation of cyclosporine therapy. (b) Twelve months after cyclosporine therapy. After 12 months of cyclosporine maintenance therapy, the patient remained asymptomatic, without ascites or hepatosplenomegaly.
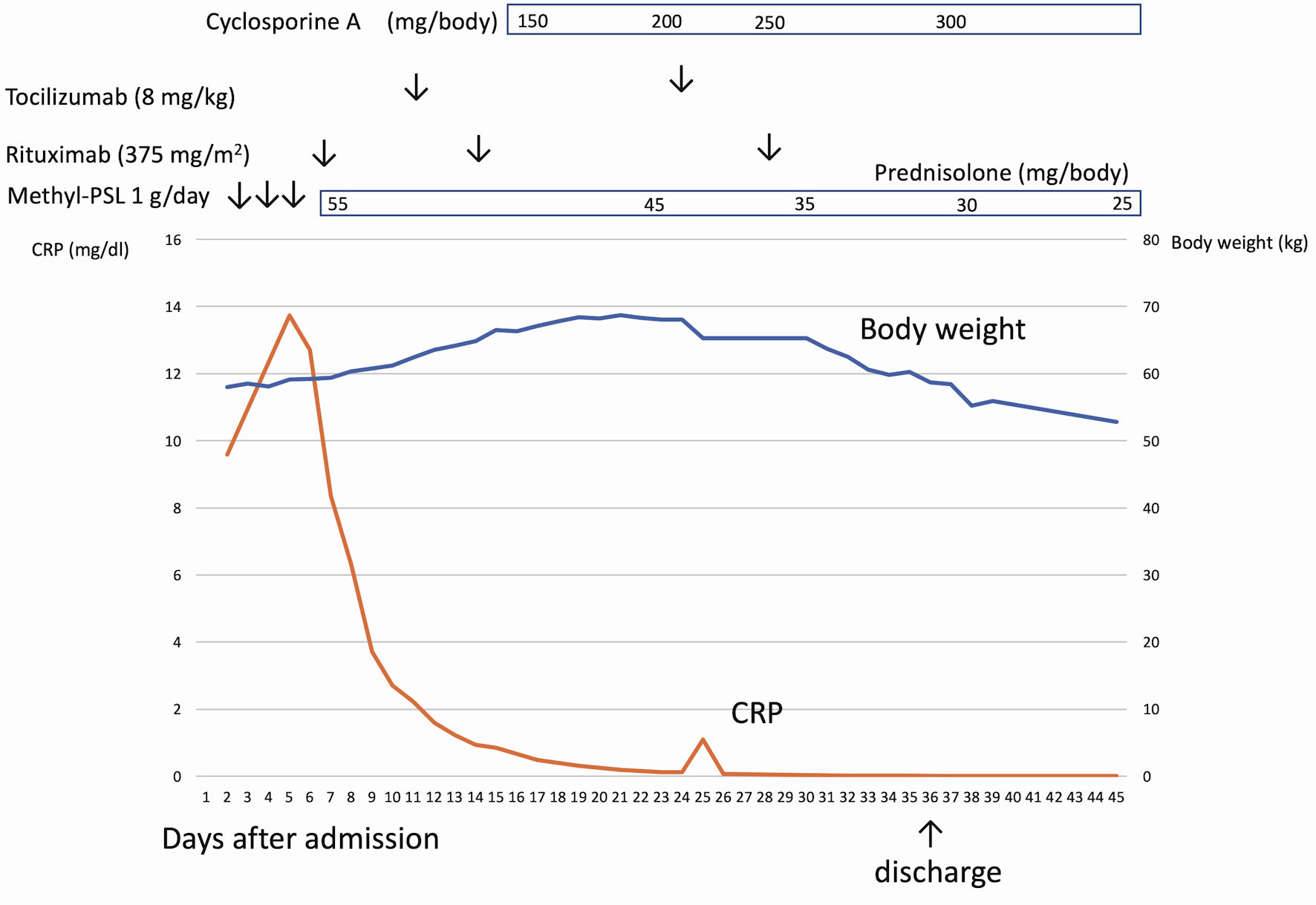
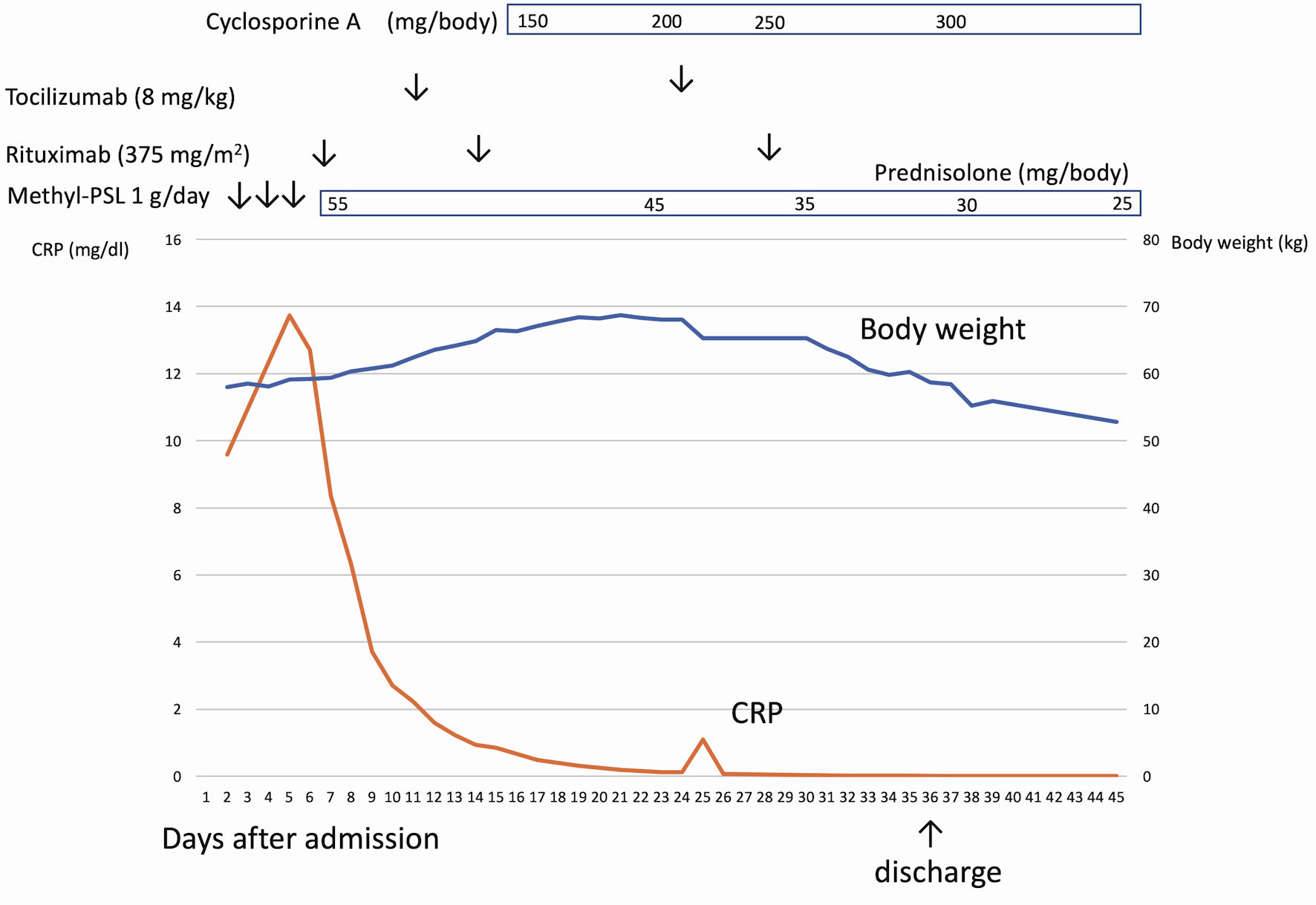
Figure 2. The clinical course of case 1. After admission, the patient had a continuous high fever and anasarca. After rituximab infusion, C-reactive protein (CRP) was normalized, but anasarca worsened. Cyclosporine was administered to the patient, which successfully resolved anasarca and ascites.
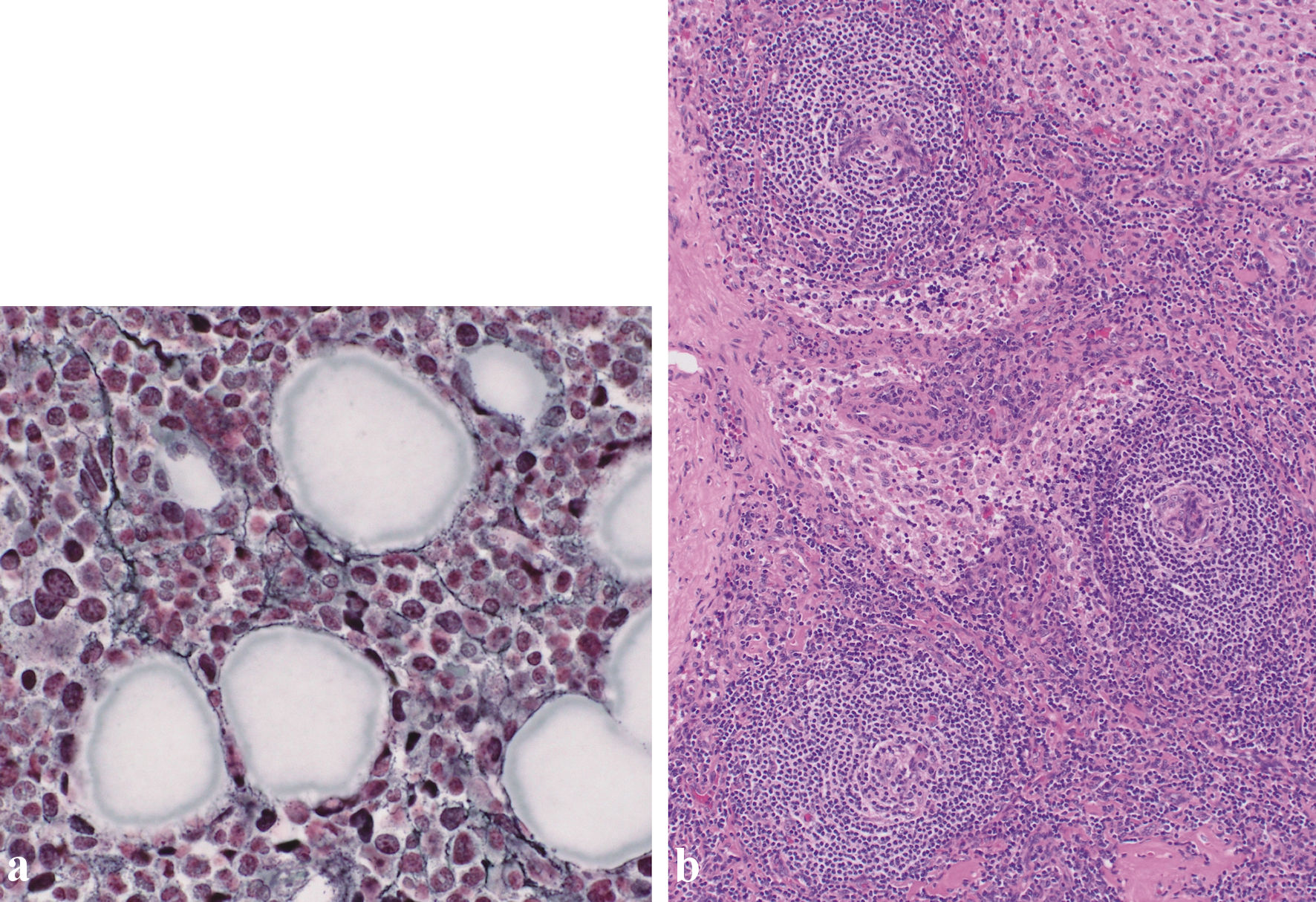
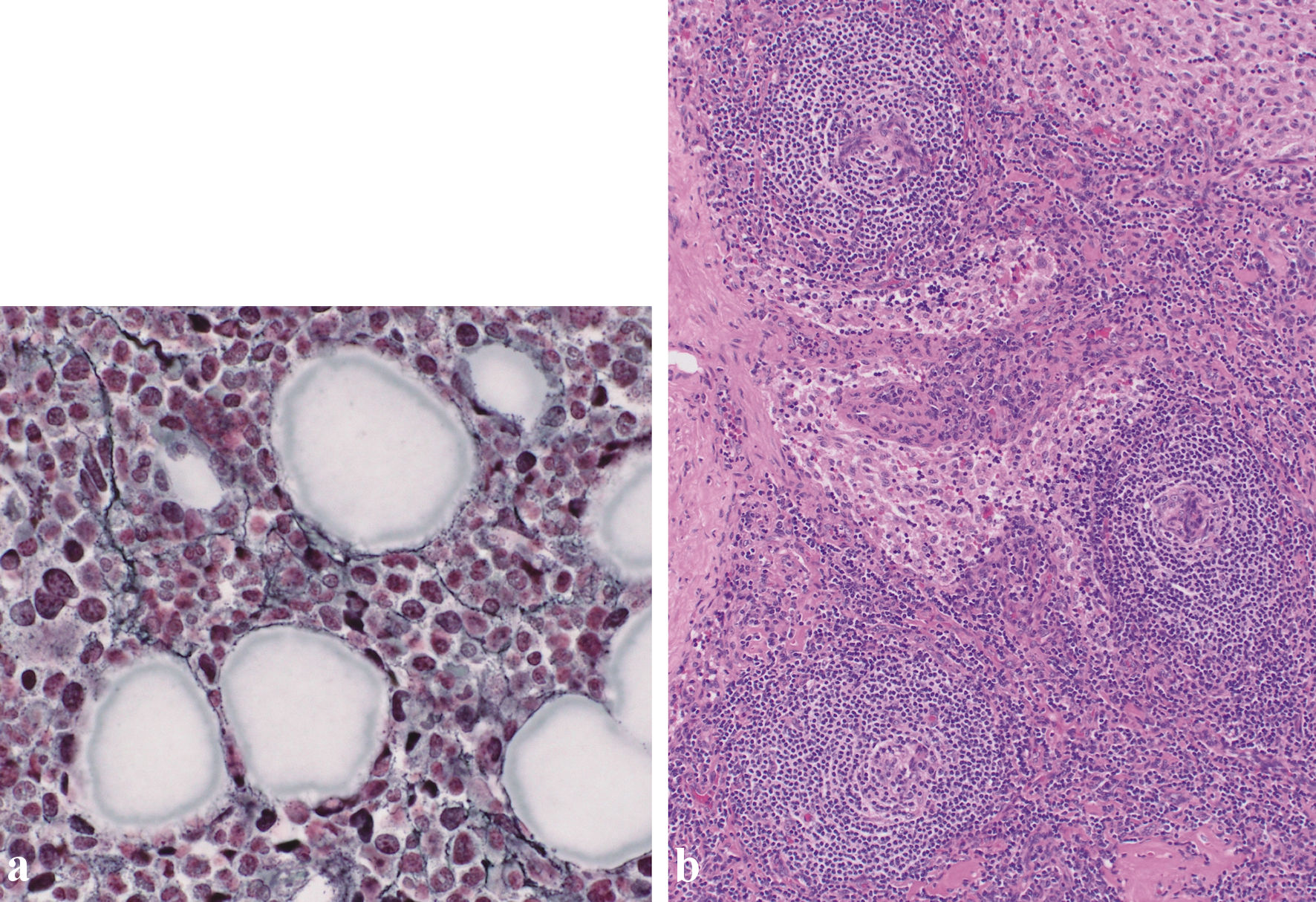
Figure 3. (a) Silver staining of the bone marrow revealed a network of reticulin fibers (original magnification × 400). (b) Biopsy of the right inguinal lymph node. Biopsy of the right inguinal lymph node (hematoxylin and eosin staining) revealed enlarged endothelial cell nuclei with proliferation of venules in the atrophied germinal centers. Plasma cell infiltration is observed in the intrafollicular zone (original magnification × 100).
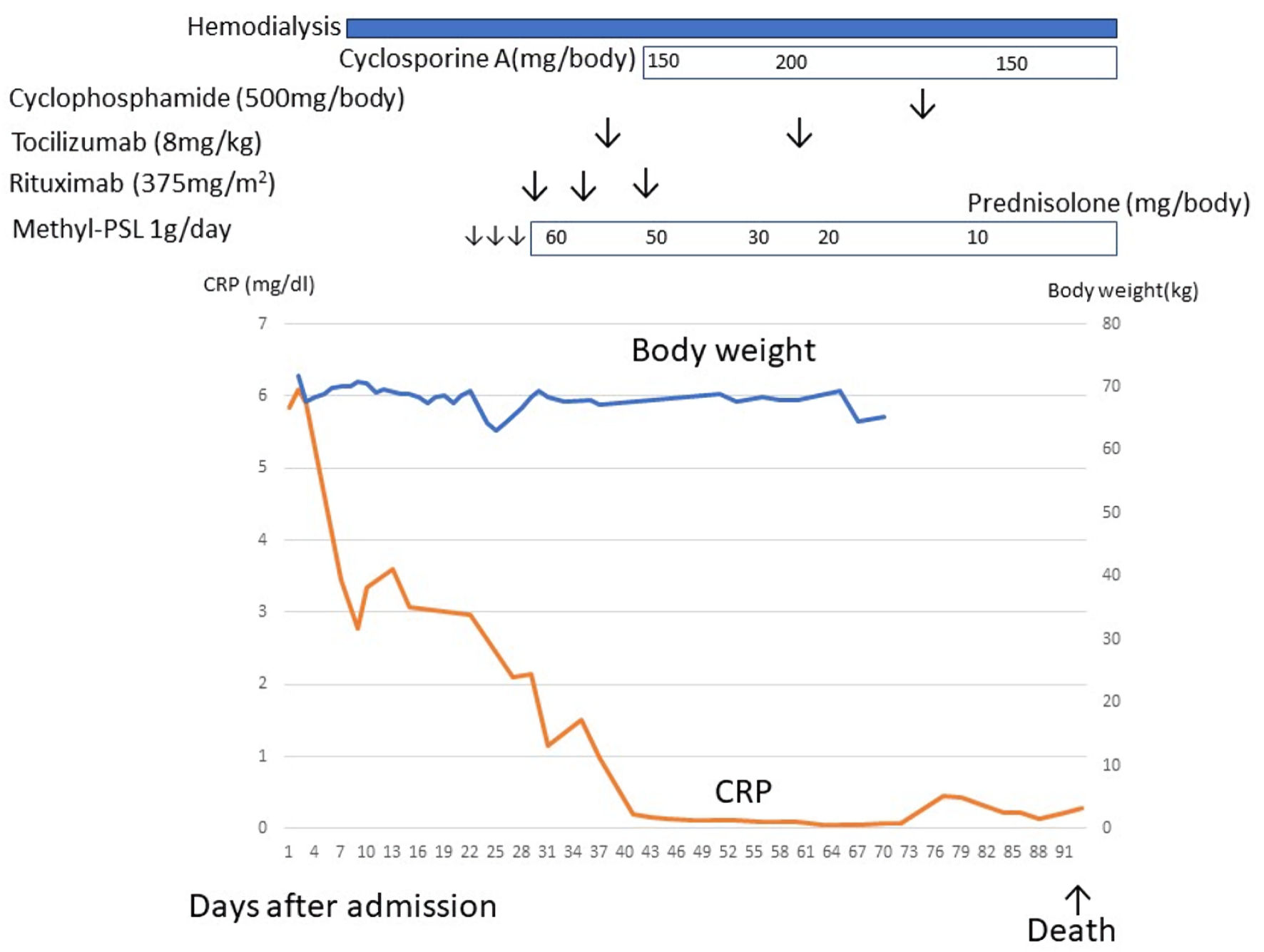
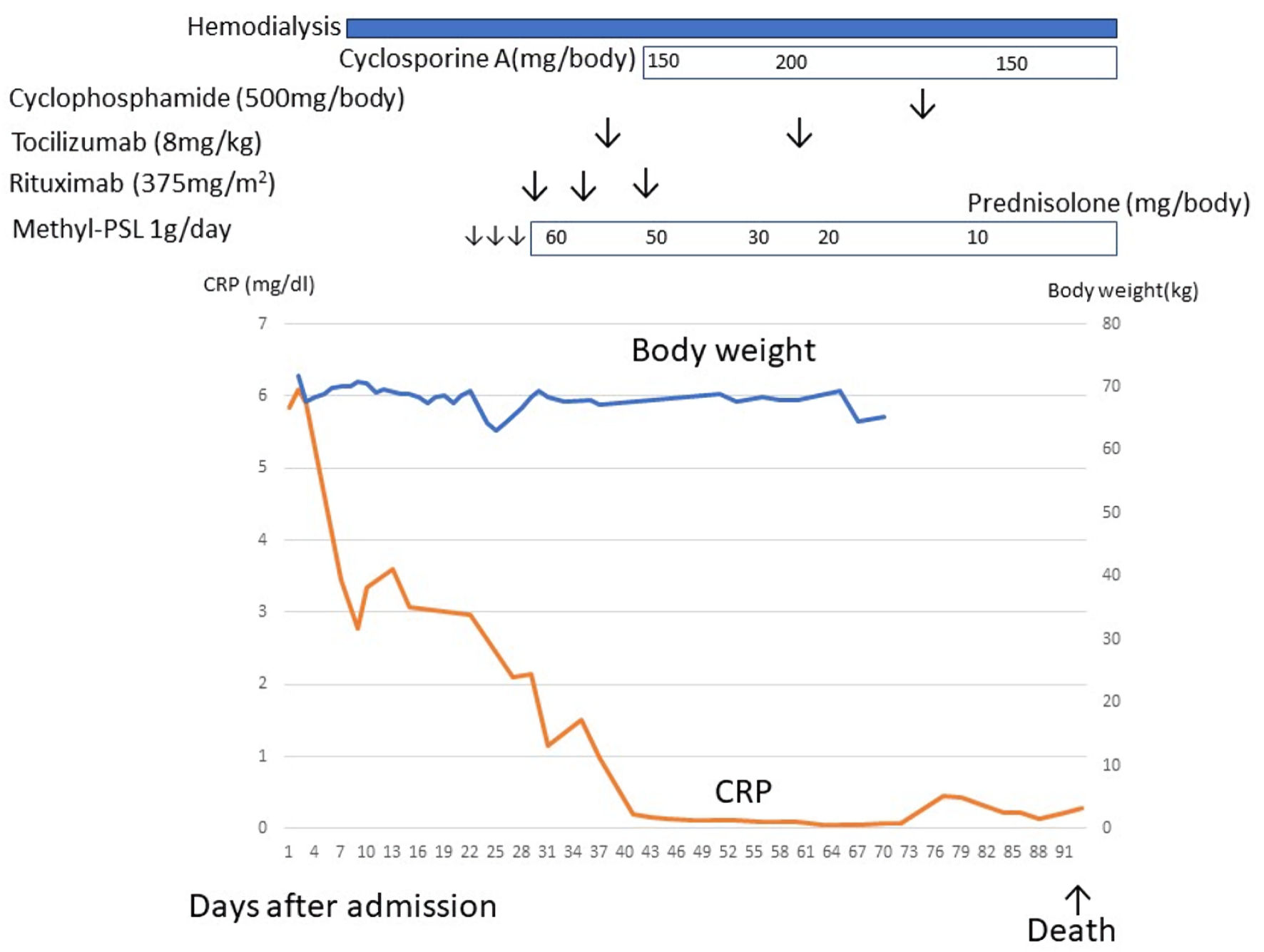
Figure 4. The clinical course of case 2. After admission, the patient developed severe ascites and renal dysfunction. Renal dysfunction did not respond to diuretics, and hemodialysis was indicated. After a diagnosis of TAFRO syndrome, methylprednisolone, rituximab, tocilizumab, and cyclosporine, cyclophosphamide therapy was initiated but ineffective. This patient died due to herpes zoster encephalitis. CRP: C-reactive protein.
Tables
Table 1. Diagnostic Criteria of TAFRO Syndrome
| Diagnostic criteria | Case 1 | Case 2 |
|---|
| A diagnosis of TAFRO syndrome requires all three major categories and at least two of four minor categories. Malignancies, autoimmune disorders, infectious disorders, POEMS syndrome, hepatic cirrhosis, and thrombotic thrombocytopenic purpura/hemolytic uremic syndrome were excluded. |
| Major categories | | |
| Anasarca | + | + |
| Thrombocytopenia | + | + |
| Systemic inflammation | + | + |
| Minor categories | + | + |
| Castleman disease-like features on lymph node biopsy | + | + |
| Reticulin myelofibrosis | + | + |
| Mild organomegaly | + | + |
| Progressive renal insufficiency | + | + |
Table 2. Laboratory Data of Case 1 and Case 2
| Laboratory data | Case 1 | Case 2 | Reference ranges |
|---|
| WBC: white blood cell count; Hb: hemoglobin; Plt: platelet count; AST: aspartate aminotransferase; ALT: alanine aminotransferase; γ-GTP: γ-glutamyl transpeptidase; ALP: alkaline phosphatase; CRP: C-reactive protein; IgG: immunoglobulin G; IL-6: interleukin-6; VEGF: vascular endothelial growth factor; PT-INR: prothrombin time-international normalized ratio; APTT: activated partial thromboplastin time; FDP: fibrin degradation product. |
| WBC (/µL) | 8,780 | 5,740 | 3,300 - 8,600 |
| Hb (g/dL) | 10.1 | 11.0 | 13.7 - 16.8 |
| Plt (/µL) | 56,000 | 67,000 | 158,000 - 348,000 |
| AST (U/L) | 13 | 25 | 13 - 30 |
| ALT (U/L) | 7 | 7 | 10 - 42 |
| γ-GTP (U/L) | 82 | 12 | 13 - 64 |
| ALP (U/L) | 628 | 148 | 106 - 322 |
| Creatinine (mg/dL) | 1.7 | 2.74 | 0.65 - 1.07 |
| CRP (mg/L) | 95.9 | 59.1 | < 14 |
| IgG (mg/dL) | 948 | 1187 | 861 - 1,747 |
| IL-6 (pg/mL) | 11 | 55 | < 7.0 |
| VEGF (pg/mL) | 5,791.4 | 2,566.3 | 143.1 - 658.8 |
| PT-INR | 1.13 | 1.3 | 0.9 - 1.2 |
| APTT (s) | 37.3 | 45 | 28 - 39.5 |
| FDP (µg/mL) | 43.3 | 30.4 | < 5 |