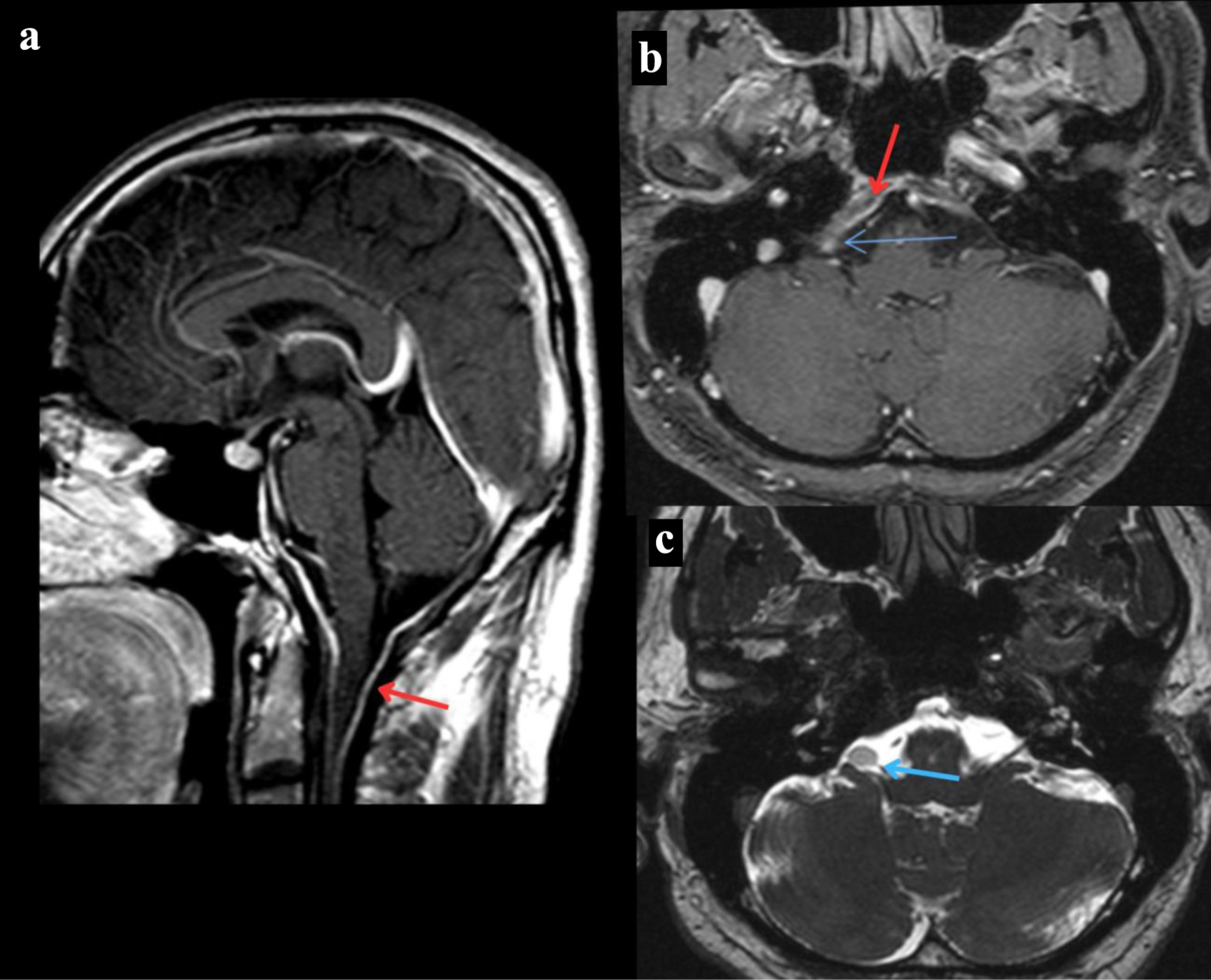
Figure 1. MRI of the brain. (a) T1-weighted MRI of the brain sagittal section post-contrast that reveals dural thickening of the posterior fossa indicated by the red arrow. (b) T1-weighted MRI of the brain axial section post-contrast that reveals a right cerebellopontine angle mass revealed by the blue arrow and dural thickening of the posterior fossa indicated by the red arrow. (c) T2-weighted MRI of the brain axial section that reveals a right cerebellopontine angle mass revealed by the blue arrow. MRI: magnetic resonance imaging.