Figures
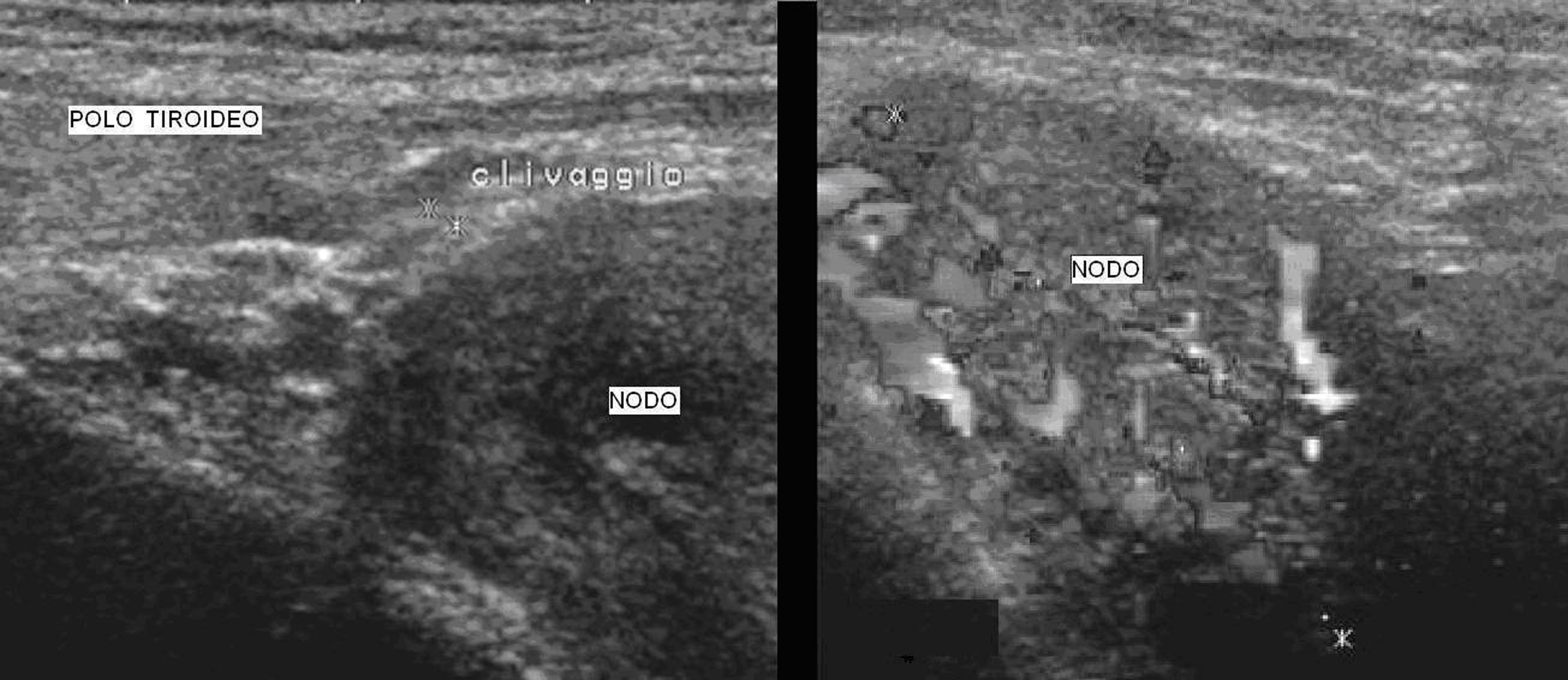
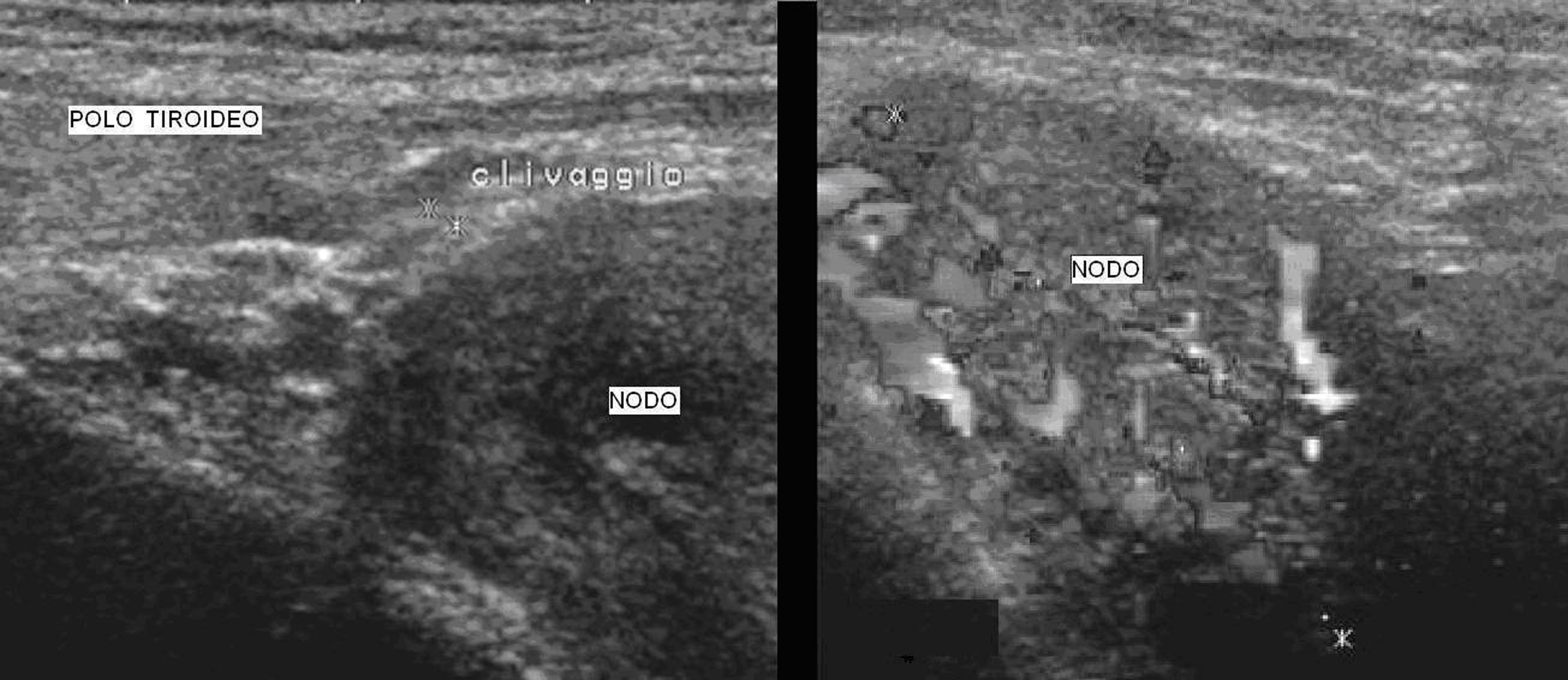
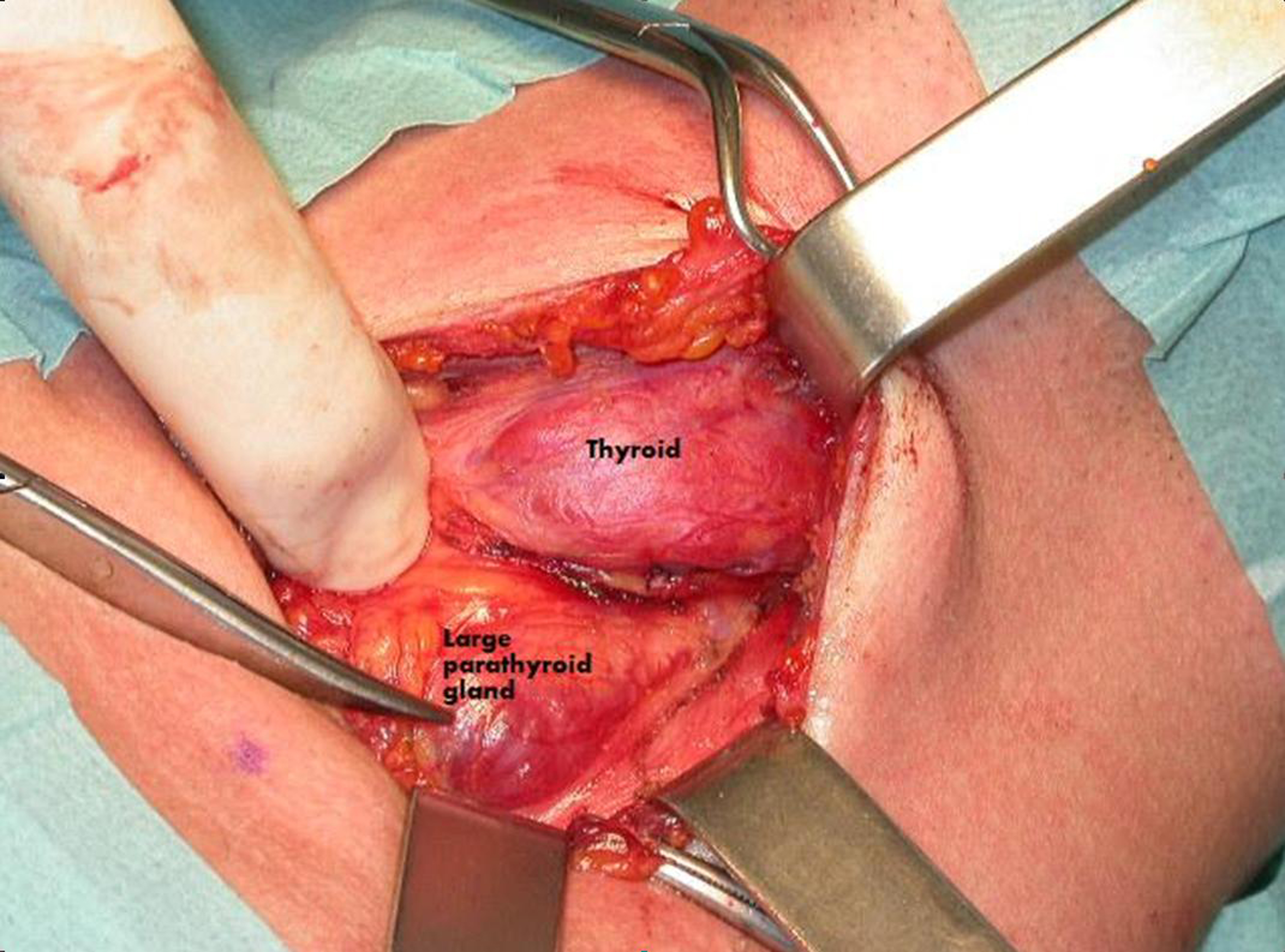
Figure 1. Ultrasonography. Ultrasound scan showed a large solid (41 x 31 x 24 mm) hypo-echogen node contiguous to the left thyroid lobe. On the right picture we could observe the high intranodal vascularisation.
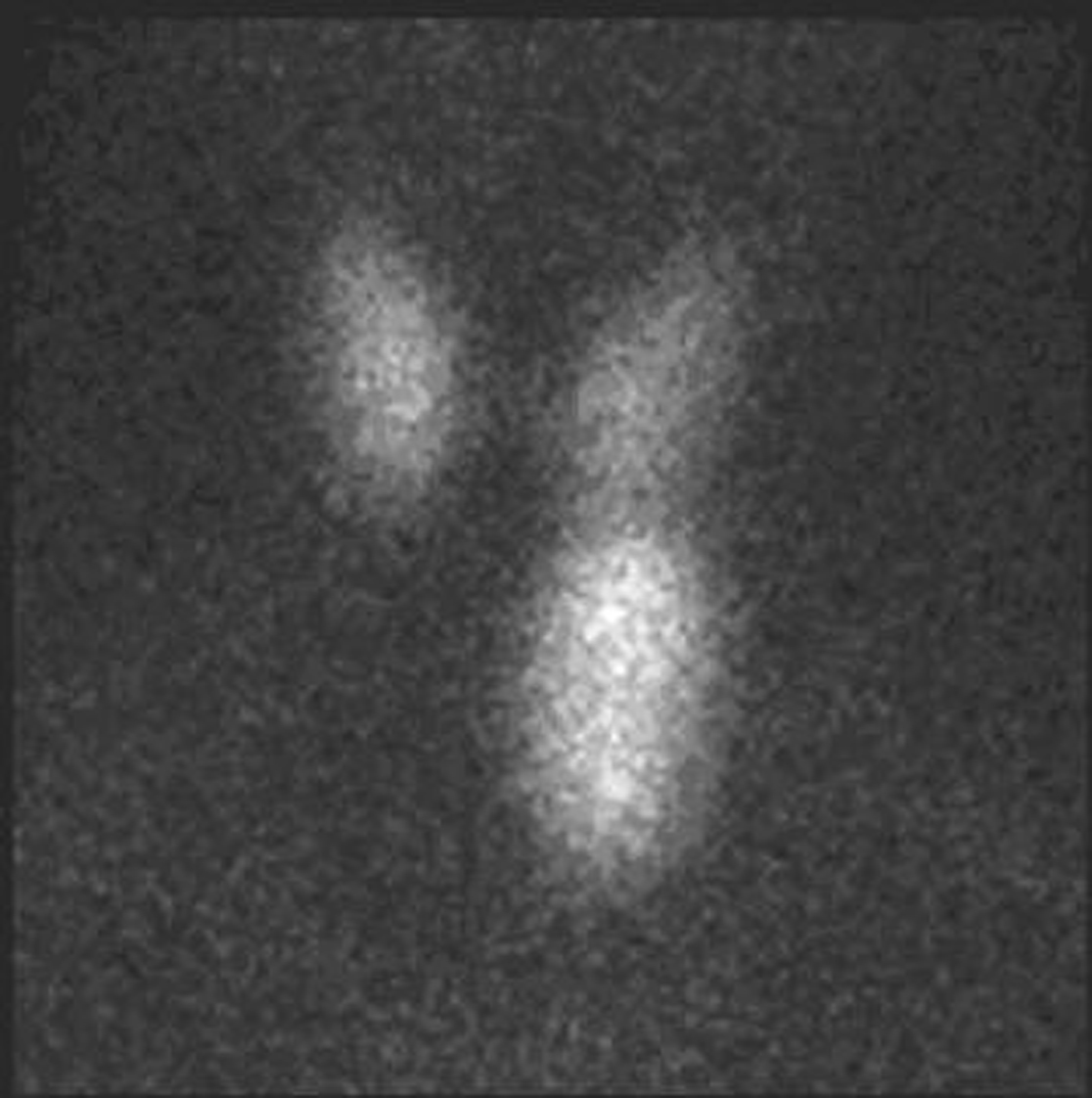
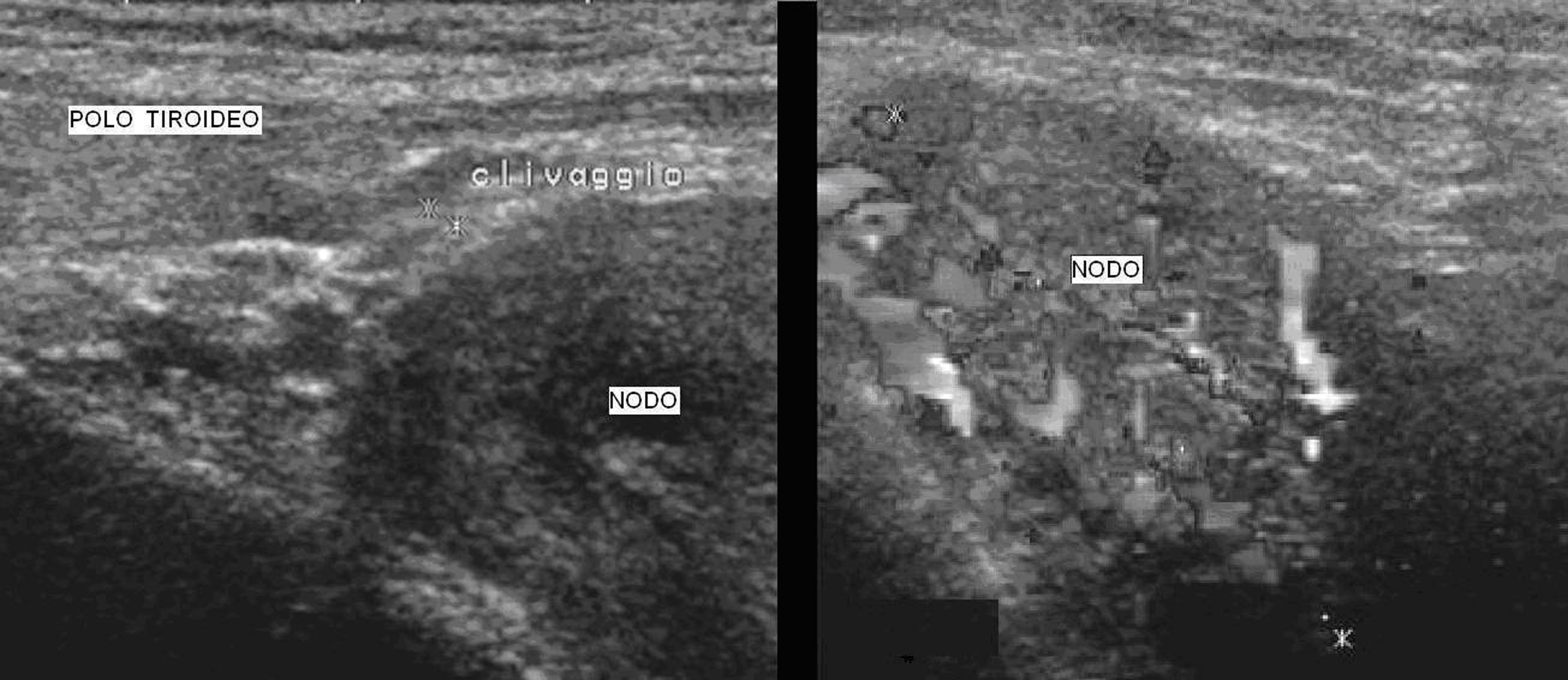
Figure 2. Thyroid scintigraphy. Tc99m-pertechnetate, that mimics iodine, is rapidly concentrated in the thyroid but conversely to iodine is quickly released from the thyroid with a half life of about one hour. While Tc99m-pertechnetate accumulates in the healthy thyroid it usually does not accumulate in the parathyroid [1].The thyroid study was obtained 15 minutes after the administration of 74 MBq of Tc99m-pertechentate. All the images were obtained with a Millennium VG gamma camera (GE Healthcare, Wisconsin, USA) using a LEHR collimator. Thyroid scintigraphy using Tc99m-pertechnetate showed a large intense uptake of tracer in the left lower pole of the thyroid.
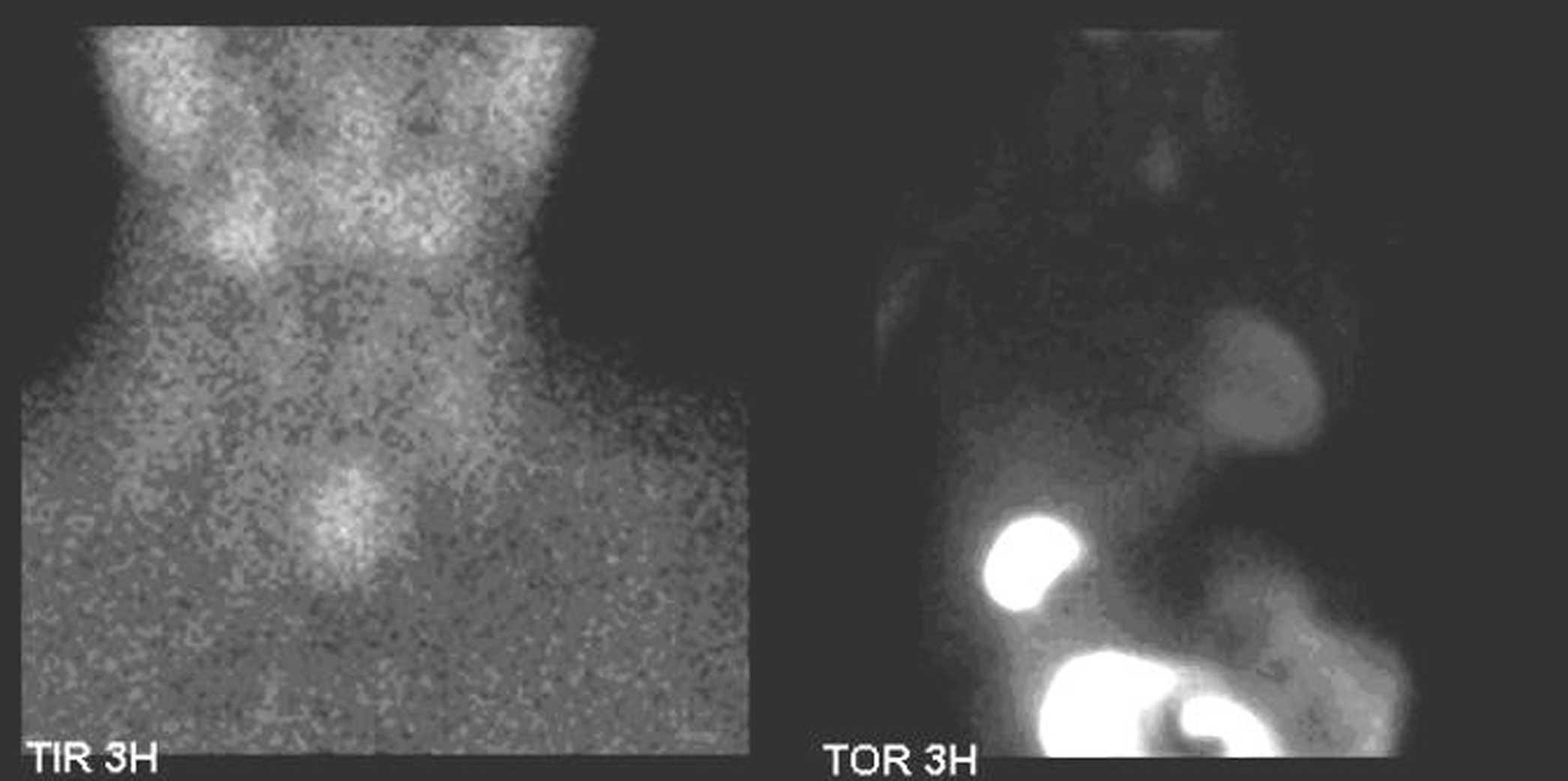
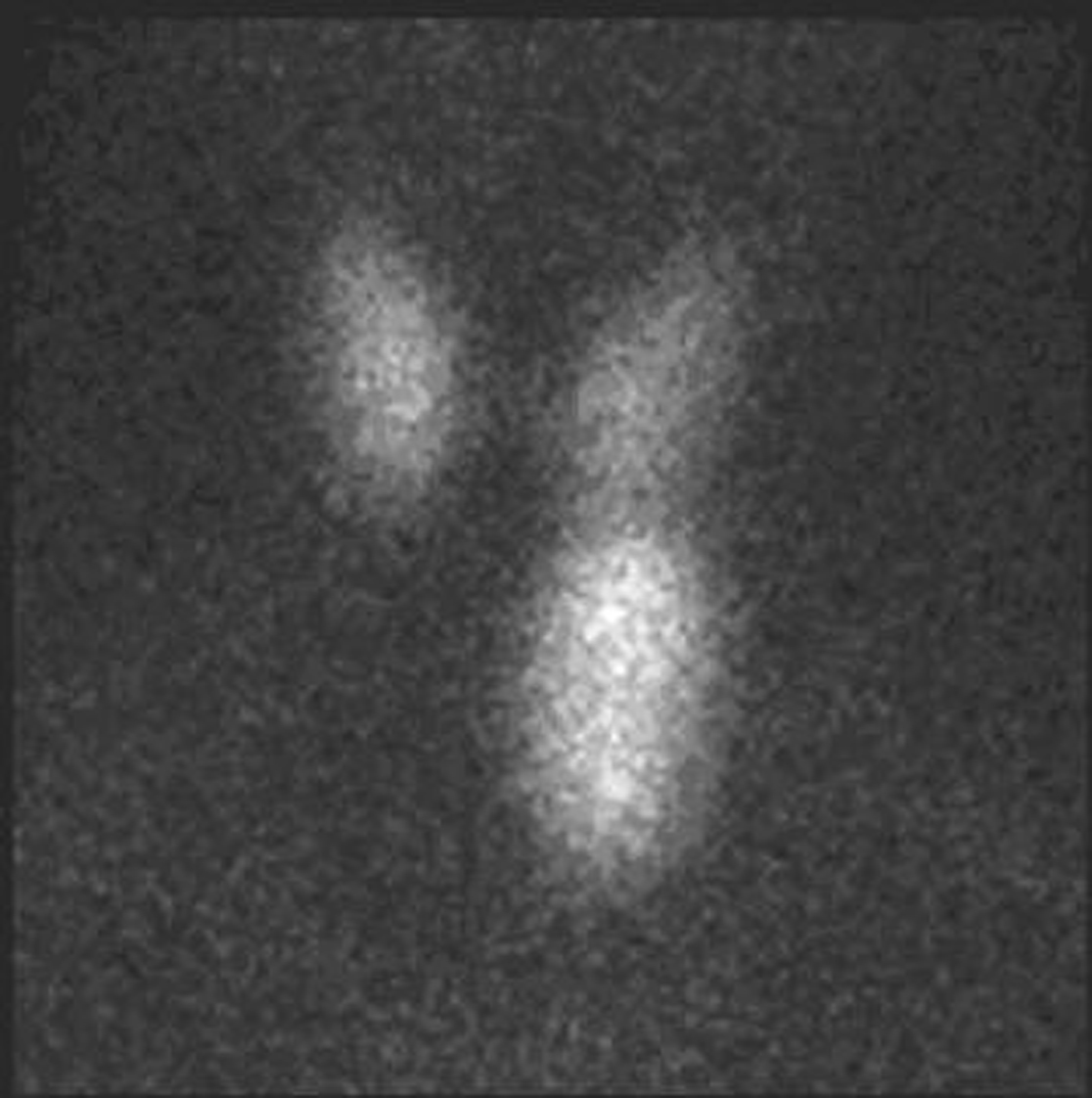
Figure 3. Parathyroid scintigraphy. SestaMIBI is a monovalent lipophilic cation that diffuses passively across cell membranes, concentrates in mitochondria and accumulates in adenomatous parathyroid tissue because of increased blood supply, higher metabolic activity and the absence of glycoprotein on the cell membrane [2]. Parathyroid scintigraphy was performed immediately after thyroid scintigraphy and the patient was given 740 MBq of Tc99m-sestaMIBI followed by 600 mg of sodium perchlorate for thyroid blocking. Additional anterior images of the neck were acquired 20 minutes and 3 hours after, followed then by a late chest image. All the images were obtained with a Millennium VG gamma camera (GE Healthcare, Wisconsin, USA) using a LEHR collimator. Parathyroid scintigraphy using sestaMIBI showed an intense and persistent uptake on the tracer in the left lower left pole of the thyroid. No other focus of uptake was found in the chest image.
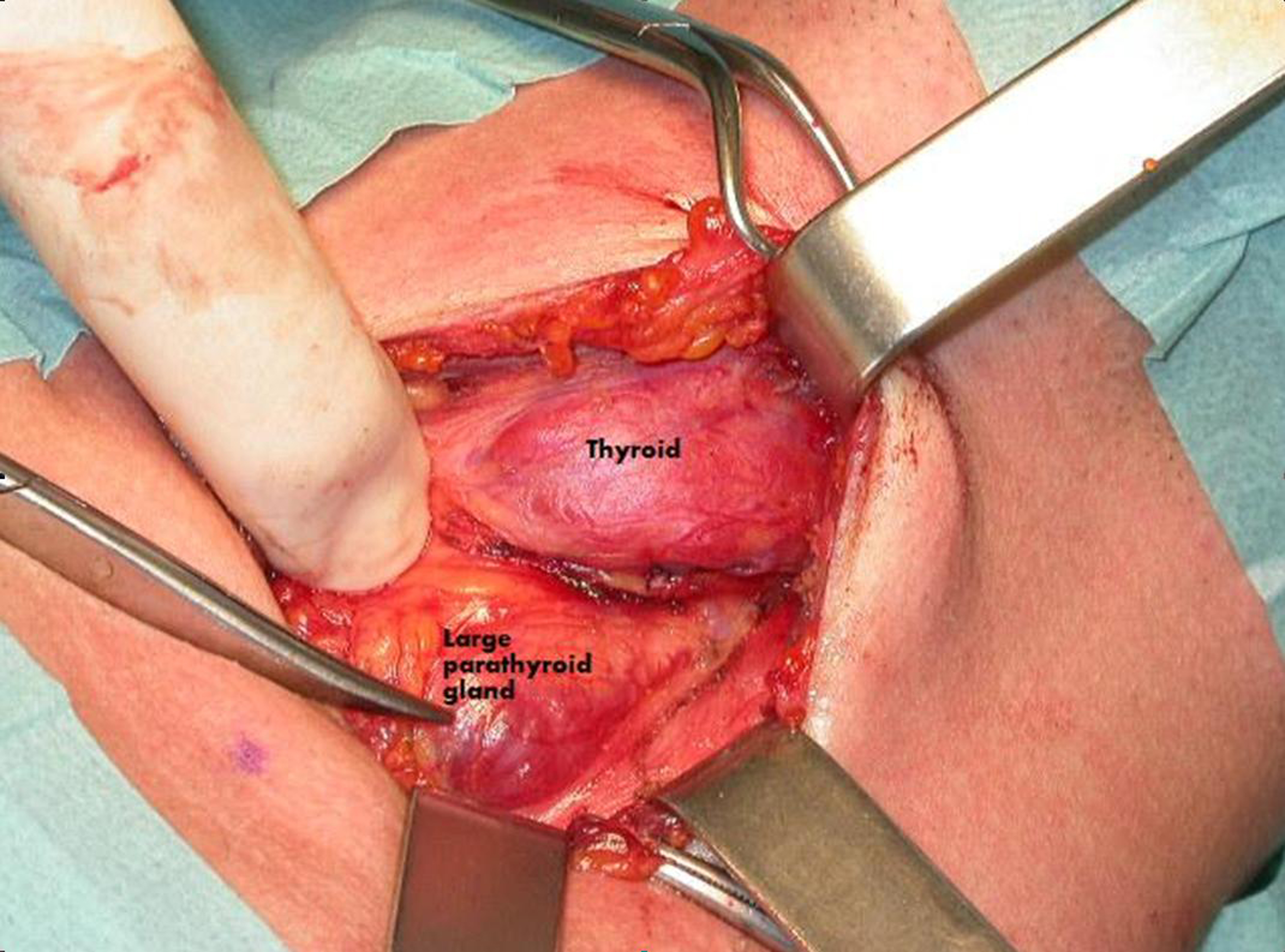
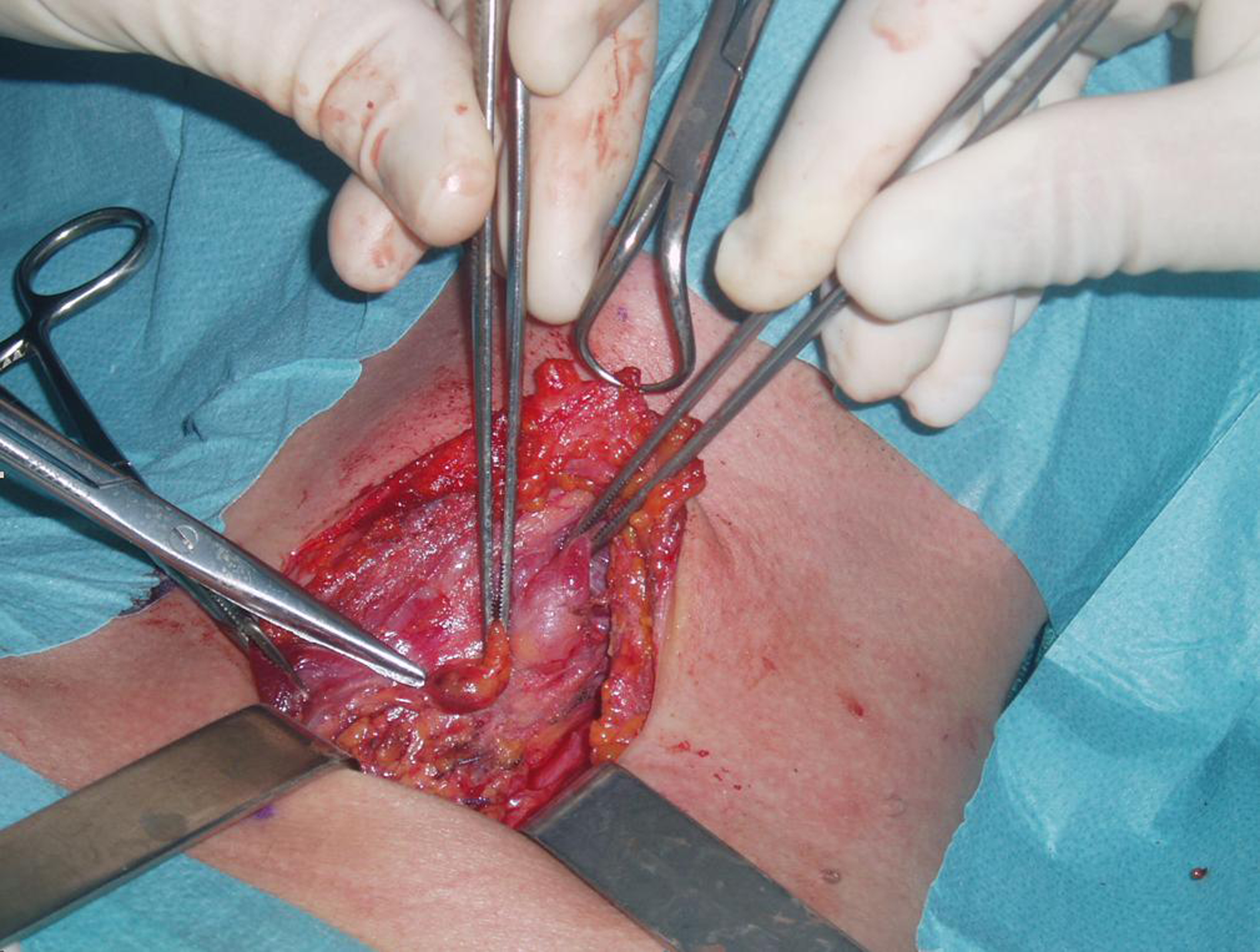
Figure 4. Surgical procedure. During surgery a large parathyroid gland was identified near the left thyroid lobe.

Figure 5. Excised parathyroid gland. The large (45 x 30 x 25 mm) superior left parathyroid gland was excised and afterwards diagnosed as an adenoma.
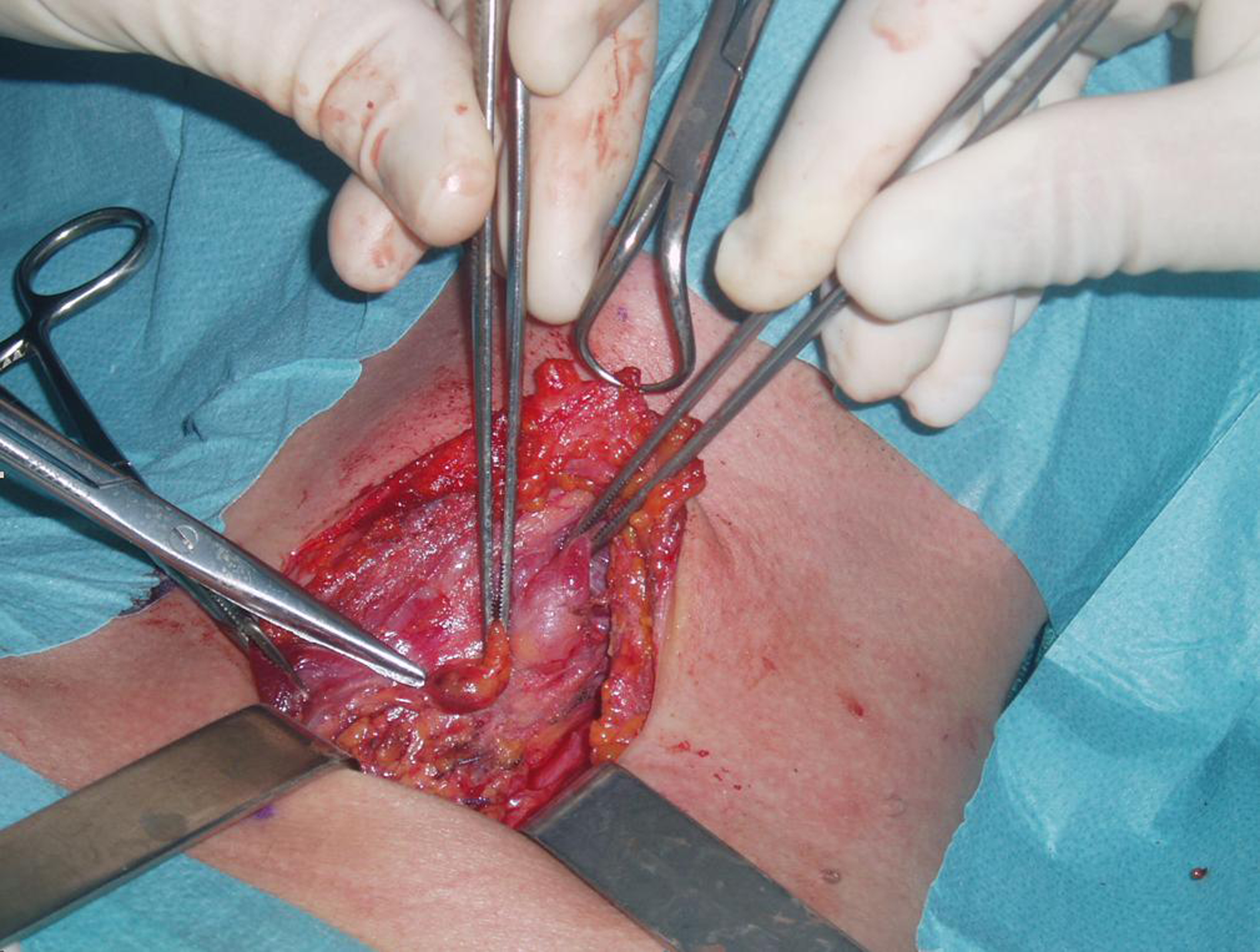
Figure 6. Normal parathyroid gland. The lower left parathyroid gland was grossly normal and therefore was not excised also because PHT decreased abruptly during surgical intervention.
Table
Table 1. Different Patterns of Radiopharmaceuticals Uptake
| Pattern | Uptake in Parathyroid Adenoma |
|---|
| Tc99m-SestaMIBI | Tc99m-pertechnetate |
|---|
| Early | Late |
|---|
| 1 (usual) | Yes | Yes | No |
| 2 (not frequent) | Yes | No | No |
| 3 (not frequent) | No | Yes | No |
| 4 (hardly ever) | Yes | Yes | Yes |