| Shah et al, 2016 [1] | 82/female | Neutropenic fevers/abdominal pain and diarrhea. CT chest with ground glass opacities | Acute myeloid leukemia (AML) on chemotherapy | No susceptibility testing available. Infection was treated with vancomycin, piperacillin-tazobactam, and ciprofloxacin. |
| 36/female | Neutropenic fevers/vomiting and diarrhea | AML on chemotherapy | Susceptible to meropenem, piperacillin-tazobactam, penicillin, and metronidazole. |
| 42/female | Neutropenic fevers/shortness of breath and cough with a nodular infiltrate on chest CT | AML on chemotherapy | Susceptibility results were only provided to metronidazole, the patient was treated empirically with piperacillin-tazobactam and then a 2-week course of clindamycin. |
| 55/male | Neutropenic fevers/lower abdominal pain and diarrhea | Myelodysplastic syndrome (MDS) on chemotherapy | No subspeciality testing available. Initially treated with cefepime, followed by vancomycin and piperacillin-tazobactam. |
| 60/male | Neutropenic fevers/shortness of breath and cough and a new perihilar infiltrate on chest X-rays | AML on chemotherapy | No susceptibility testing available. Initially treated with cefepime, followed by a 2-week course of vancomycin and metronidazole. |
| 69/male | Neutropenic fevers with ground-glass opacities on chest CT imaging | MDS on chemotherapy | No susceptibility testing available. Initially treated with vancomycin and cefepime followed by piperacillin-tazobactam for 2 weeks. |
| 60/male | Neutropenic fevers/fatigue | AML on chemotherapy | No susceptibility testing available. Initially treated with ciprofloxacin, then switched to vancomycin and cefepime with cultures results. |
| Miller et al, 2001 [2] | 28/male | Abdominal pain, vomiting, and watery diarrhea. CT abdomen with Crohn’s features. Colonoscopy and biopsy confirmed CD. Blood cultures grew C. tertium | CD | No susceptibility testing available. Empirically treated with ciprofloxacin and clindamycin. |
| Miller et al, 2001 [2] | A case series of 32 patients including the above one [2]; 22 patients were males; age ranged widely from 16 to 75 years; 29 patients were neutropenic secondary to chemotherapy. Three non-neutropenic patients were as follows: one had spontaneous bacterial peritonitis (SBP) associated with alcoholic liver cirrhosis, one with CD, and the last one with systemic lupus erythematosus (SLE) treated with high-dose steroids. |
| Steyaert et al, 1999 [3] | 65/male | Neutropenic fevers/abdominal pain and diarrhea | AML on chemotherapy | Resistant to ceftazidime, cefepime, and clindamycin; intermediately resistant to penicillin; and susceptible to metronidazole, and vancomycin. Initially treated with ceftazidime and amikacin that were switched to vancomycin following sensitivity results. |
| 55/male | Neutropenic fevers/abdominal pain and diarrhea | AML on chemotherapy | Resistant to ceftazidime, cefepime, and clindamycin; intermediately resistant to penicillin; and susceptible to metronidazole, quinolones, and vancomycin. He was treated with vancomycin. |
| Wazir et al, 2019 [4] | 62/male | Fatigue and high-grade fevers in a patient with end-stage liver disease. Ascitic fluid analysis revealed SBP. Blood cultures grew C. tertium | Alcoholic liver cirrhosis | Susceptible to meropenem, metronidazole, and penicillin. Initial empiric treatment with meropenem and vancomycin then targeted meropenem therapy for 9 days with clearance of C. tertium bacteremia. |
| Sutton et al, 2017 [5] | 60/male | Worsening abdominal pain and fevers in the setting of chronic liver disease. Ascitic fluids culture isolated C. tertium | Alcoholic liver cirrhosis | Susceptible to meropenem, ciprofloxacin, clindamycin, and vancomycin. Initial empiric treatment with vancomycin and meropenem, then the latter was switched to ciprofloxacin and metronidazole. Repeat cultures were negative. |
| Chalhoub et al, 2016 [6] | 54/female | Pancolitis progressed to septic shock with acute respiratory distress syndrome (ARDS). Serial blood cultures grew C. tertium | Colitis without evidence of IBD. Probable intestinal mucosal injury triggering C. tertium translocation | Susceptible to penicillin and vancomycin, resistant to clindamycin. Initially treated imipenem, vancomycin, and ciprofloxacin, the latter switched to ampicillin. The three-antibiotics regime was continued for 3 weeks with clearance of infection. |
| Gosbell et al, 1996 [7] | 19/female | Recurrent neutropenic fevers | Acute lymphoblastic leukemia (ALL) on chemotherapy | Susceptible to penicillin, metronidazole, and vancomycin. |
| 57/female | Vomiting and diarrhea in a patient with a known history of UC | UC | No susceptibility testing available. C. tertium was isolated in the setting of polymicrobial isolates. |
| Coleman et al, 1993 [8] | 15/female | Neutropenic fevers/abdominal pain and diarrhea. CT abdomen showing enterocolitis of the cecum and right colon | ALL on chemotherapy | No susceptibility testing available. Initially treated with ceftazidime, metronidazole, and gentamicin regime switched to ciprofloxacin and vancomycin when cultures grew C. tertium. Operative intervention with right hemicolectomy was indicated to control sepsis. |
| Tappe et al, 2004 [9] | 51/female | Postoperative fever progressed to septic shock in the setting of ileus post-laparotomy and adhesiolysis | Paralytic ileus with probable mucosal injury secondary to ileus inducing C. tertium translocation | Susceptible to meropenem, imipenem, vancomycin, linezolid, and piperacillin-tazobactam, and resistant to penicillin, cefotaxime, clindamycin, and co-trimoxazole. |
| Milano et al, 2019 [10] | 43/male | High-grade fevers due to a giant hepatic abscess 4 weeks post-appendectomy for a perforated appendix requiring radiology-guided drainage of the abscess | Perforated appendix with polymicrobial peritonitis and bacterial translocation and the recent use of broad-spectrum antibiotics | No susceptibility testing available. C. tertium was isolated in gram-negative polymicrobial blood cultures and the drained hepatic abscess substance. He was treated with radiologically guided hepatic abscess drainage conjugated with piperacillin-tazobactam. |
| You et al, 2015 [11] | 44/female | Acute bronchopneumonia and C. tertium bacteremia identification of using 16S rRNA sequencing | Suicidal ingestion of glyphosate | Susceptible to penicillin, piperacillin/tazobactam, amoxicillin/clavulanic acid, cephalothin, cefoxitin, imipenem, and vancomycin, but resistance to cefotaxime, ceftazidime, cefepime, gentamicin, clindamycin, and metronidazole. |
| Ray et al, 2003 [12] | 58/male | Necrotizing fasciitis of distal lower extremity requiring fasciotomy | History of non-Hodgkin lymphoma status post-chemotherapy 6 months prior to presentation. Alcoholic liver disease | No susceptibility testing available. The patient was treated with imipenem, vancomycin, and metronidazole. |
| 40/male | Necrotizing fasciitis of proximal lower extremity requiring extensive fasciotomy | Motor vehicle accident with multiple lower extremities and abdominal injuries | Susceptible to penicillin, ampicillin, vancomycin, and metronidazole. |
| Salvador et al, 2013 [13] | 47/male | Breakthrough bacteremia with neutropenic fevers presenting with abdominal pain | ALL on chemotherapy | Susceptible to metronidazole and moxifloxacin but resistant to ceftriaxone. |
| Vanderhofstadt et al, 2010 [14] | 51/male | The patient was completely asymptomatic. Routine blood cultures prior to the start of induction chemotherapy revealed C. tertium bacteremia. | Relapsing AML status post bone marrow transplant who was due to start a new course of induction chemotherapy | Susceptible to penicillin, amoxicillin-clavulanic, and metronidazole. Resistant to clindamycin. |
| 23/male | Neutropenic fevers without a focus of infection | Non-Hodgkin lymphoma on chemotherapy | Sensitive to amikacin, and ceftazidime but resistant to amoxicillin-clavulanic. |
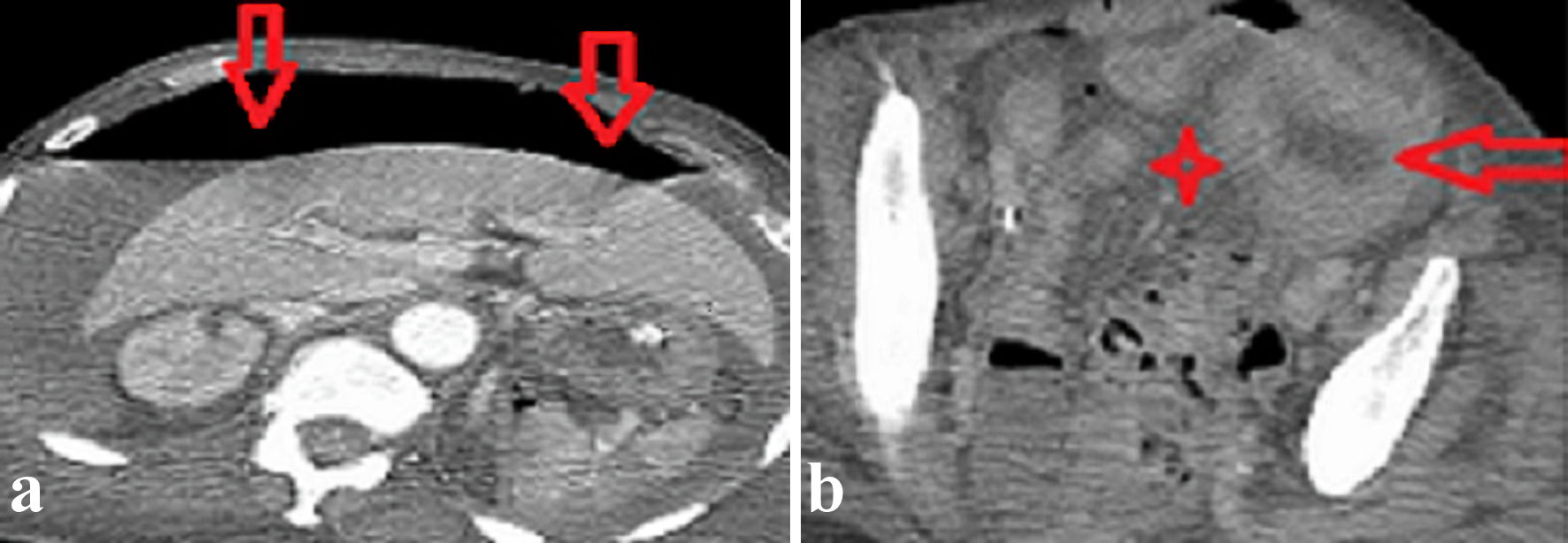
| Saad et al, 2022 (present case) | 66/female | Septic shock secondary to C. tertium bacteremia in a critically ill non-neutropenic patient with COVID-19 | Perforated colonic diverticular disease with bacterial translocation | Susceptible to meropenem, metronidazole, and amoxicillin-clavulanic, and piperacillin-tazobactam. |