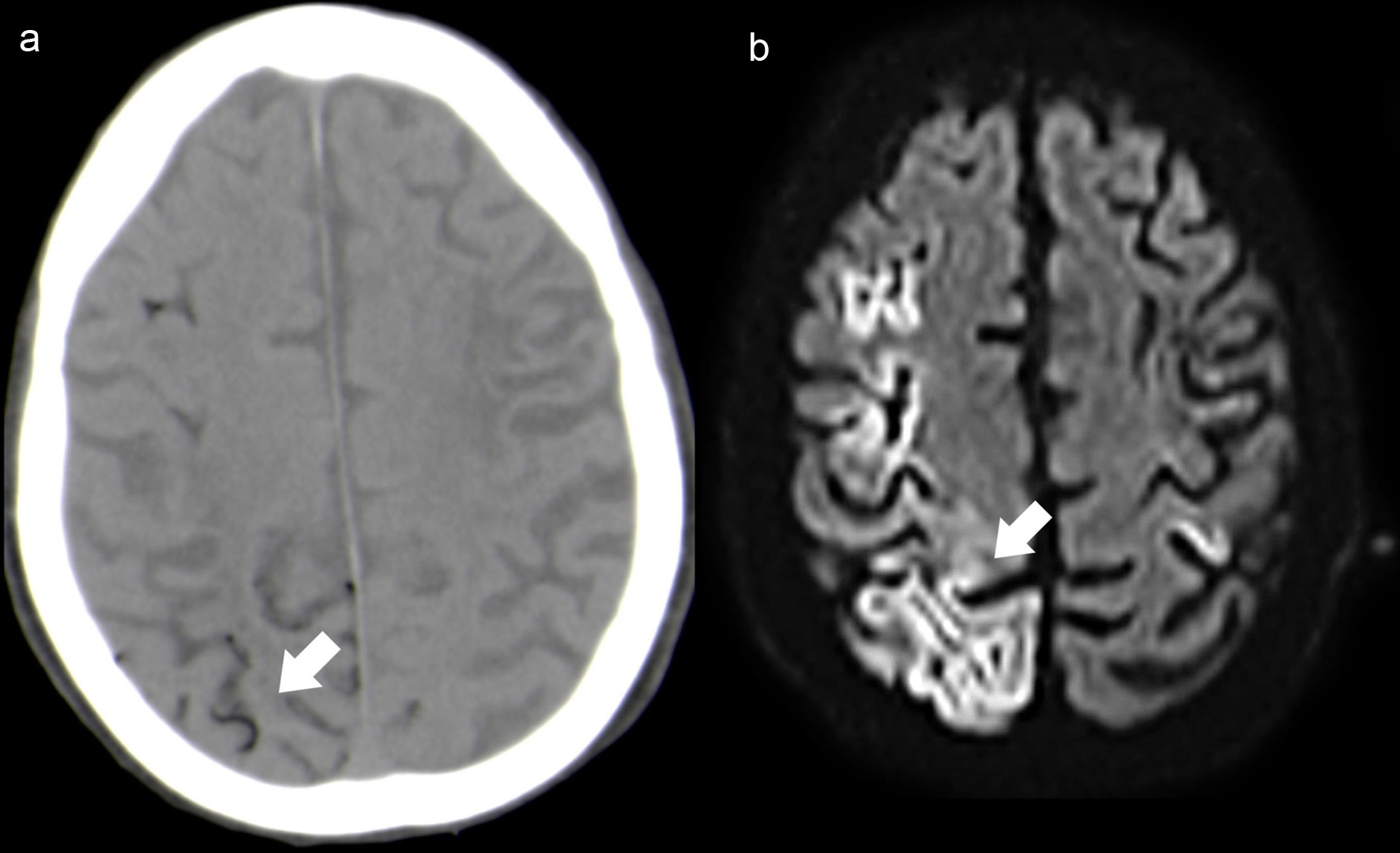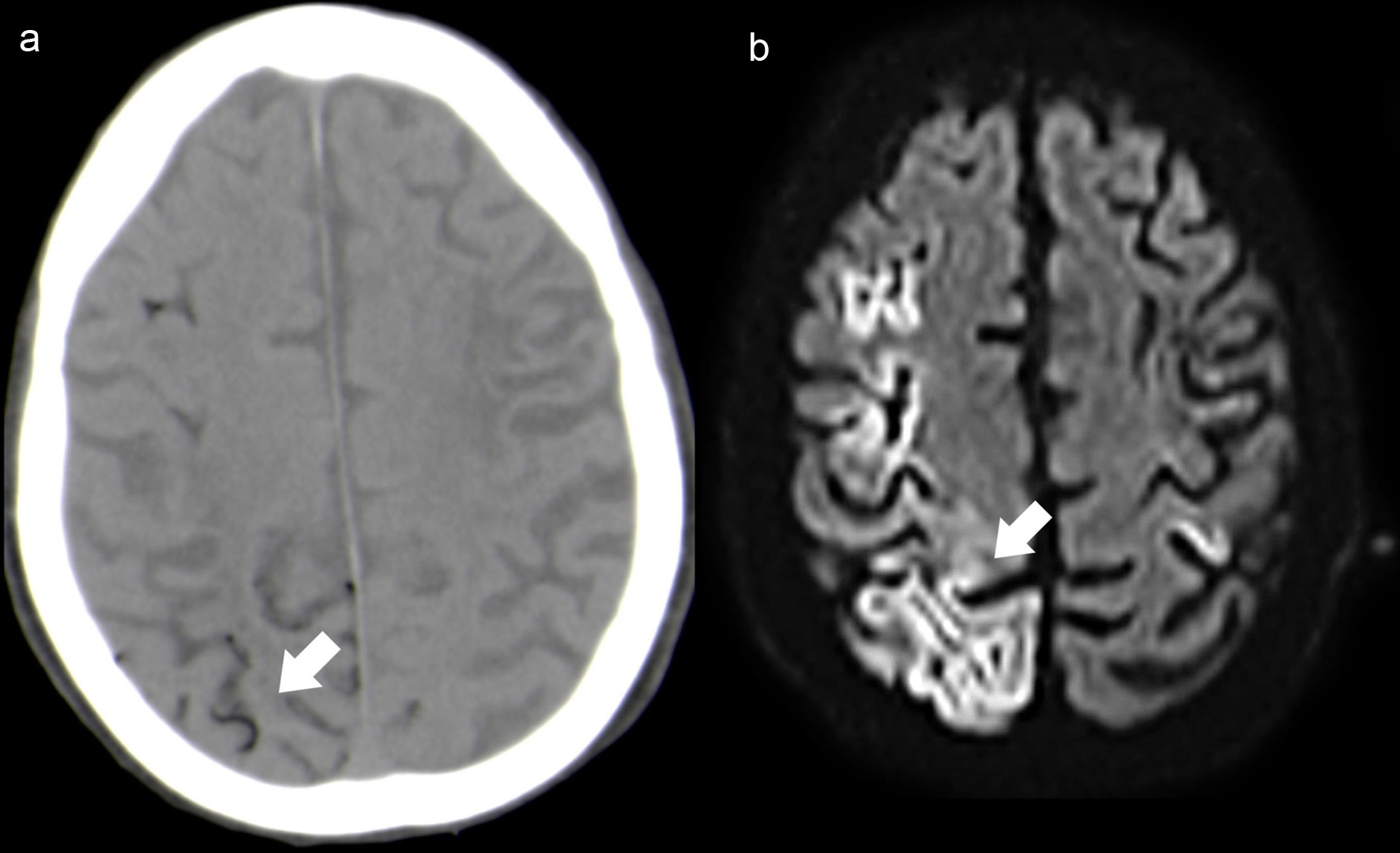
Figure 1. Case 1. Axial NCCT (a) depicts multiple small hypodense foci located mainly in the right cortical sulci (white arrow). Follow-up brain MRI (48 h after the onset), axial DWI (b) shows extensive right frontoparietal cortical ischemic lesions (white arrow), with additional small left perirolandic cortex involvement. NCCT: non-contrast computed tomography; MRI: magnetic resonance imaging; DWI: diffusion-weighted imaging.
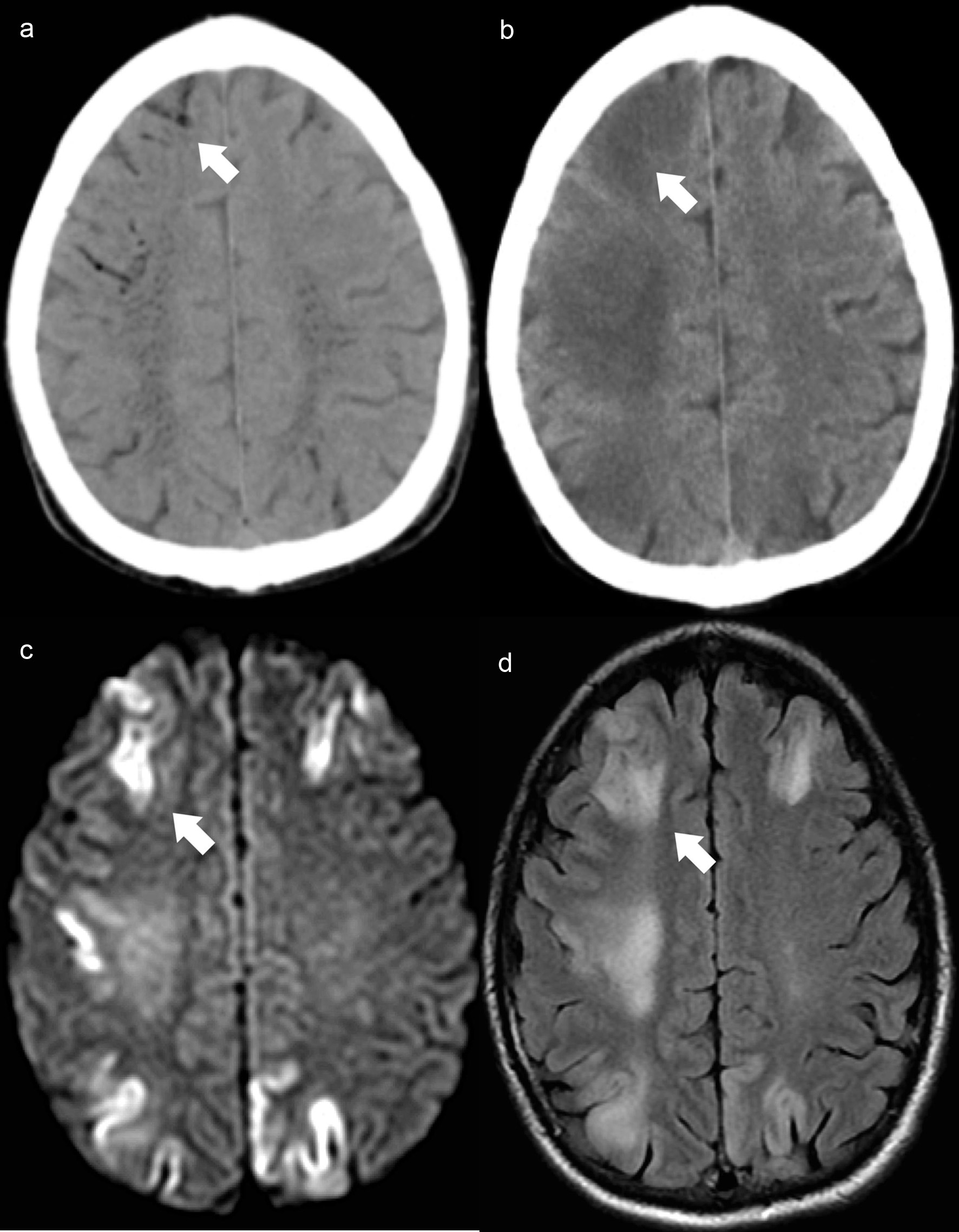
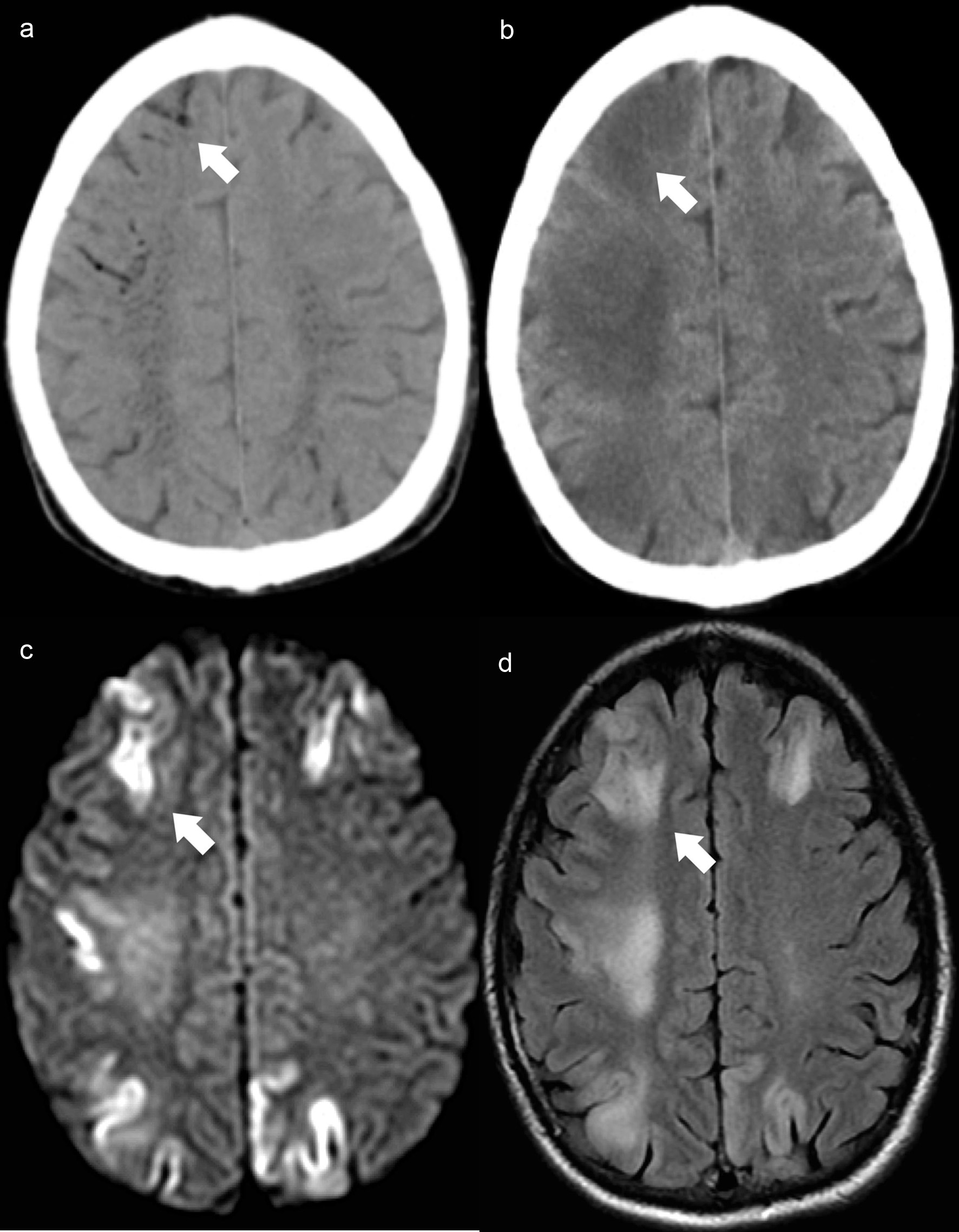
Figure 2. Case 3. Brain axial NCCT (a) demonstrates filiform air hypodensities in the high convexity sulci (white arrow) and intraparenchymal with a vascular distribution, predominantly in the semioval center. Control brain axial NCCT scan (b) reveals intracranial air reabsorption and frontoparietal cortico-subcortical dedifferentiation (white arrow). Brain MRI axial DWI (c) shows bilateral fronto-parietal cortical diffusion restriction with the corresponding cortical hyperintensity on axial FLAIR image (d) and evidence of white matter vasogenic edema (white arrow). NCCT: non-contrast computed tomography; MRI: magnetic resonance imaging; DWI: diffusion-weighted imaging; FLAIR: fluid-attenuated inversion recovery.
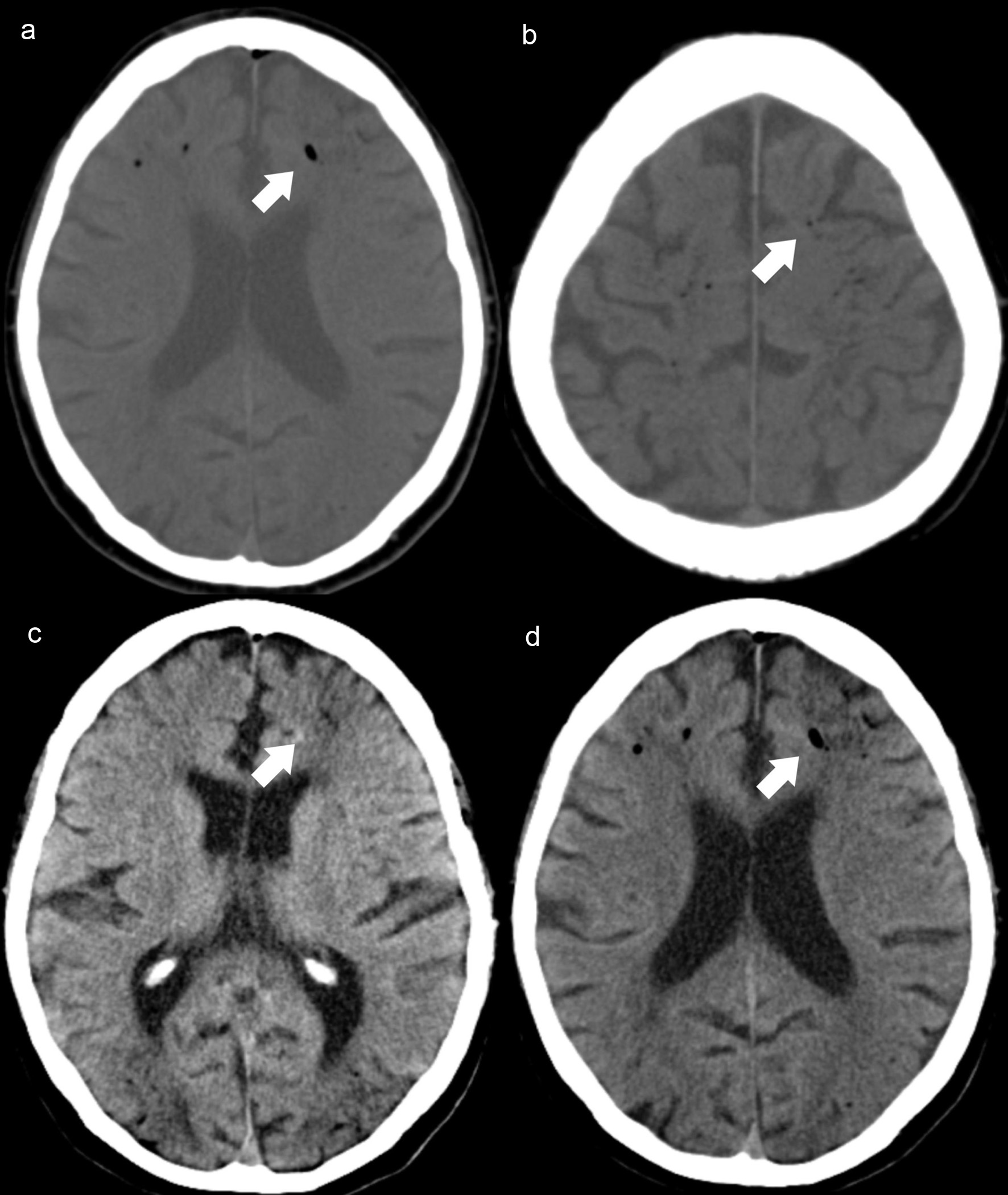
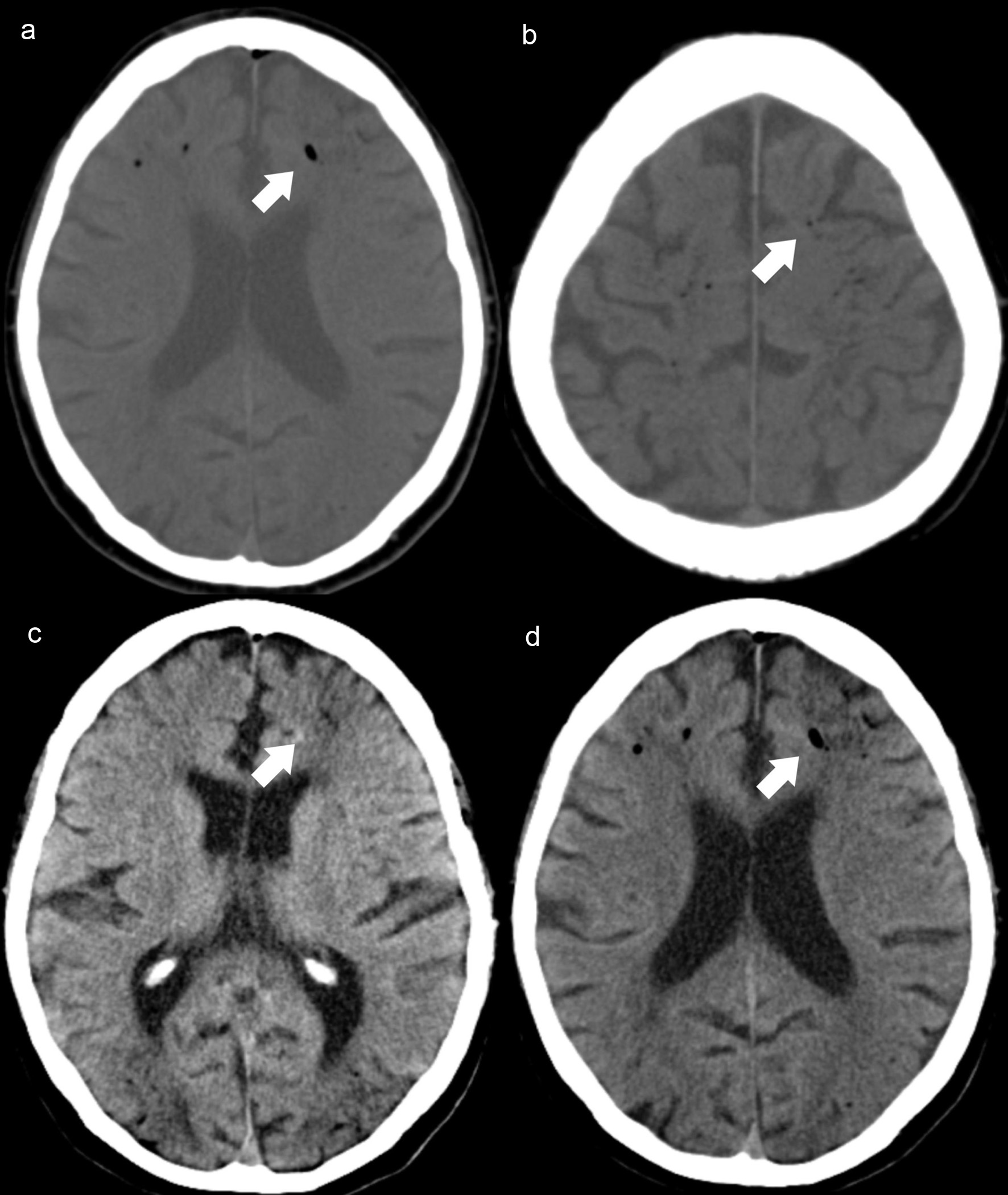
Figure 3. Case 4. Axial NCCT scan (a, b) demonstrates intracranial air, along the frontal cortical sulci (white arrows) and adjacent hypodense areas in frontal and parieto-occipital regions, revealing watershed infarcts (c, d) hypoxic-ischemic encephalopathy (white arrows). NCCT: non-contrast computed tomography.