Figures
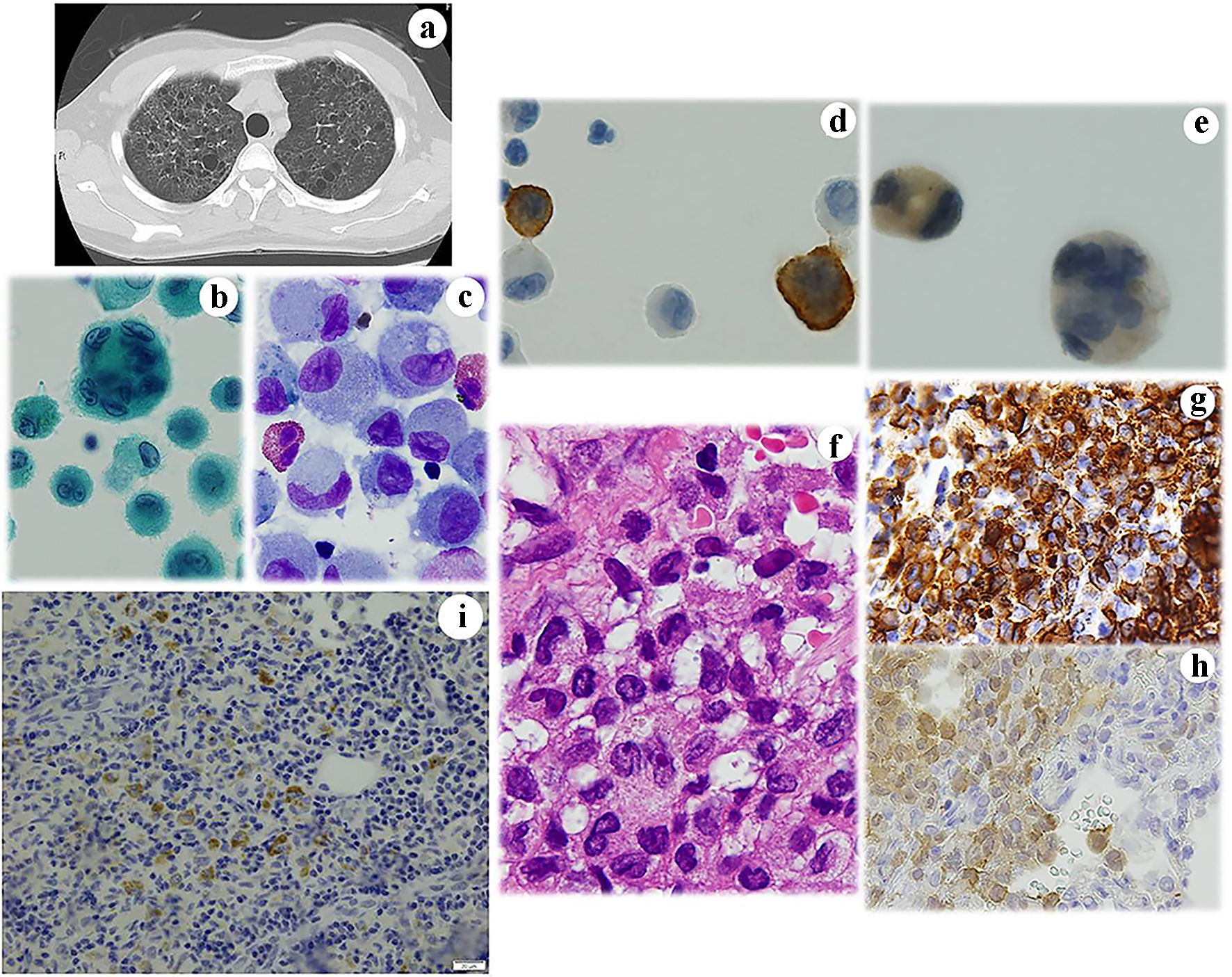
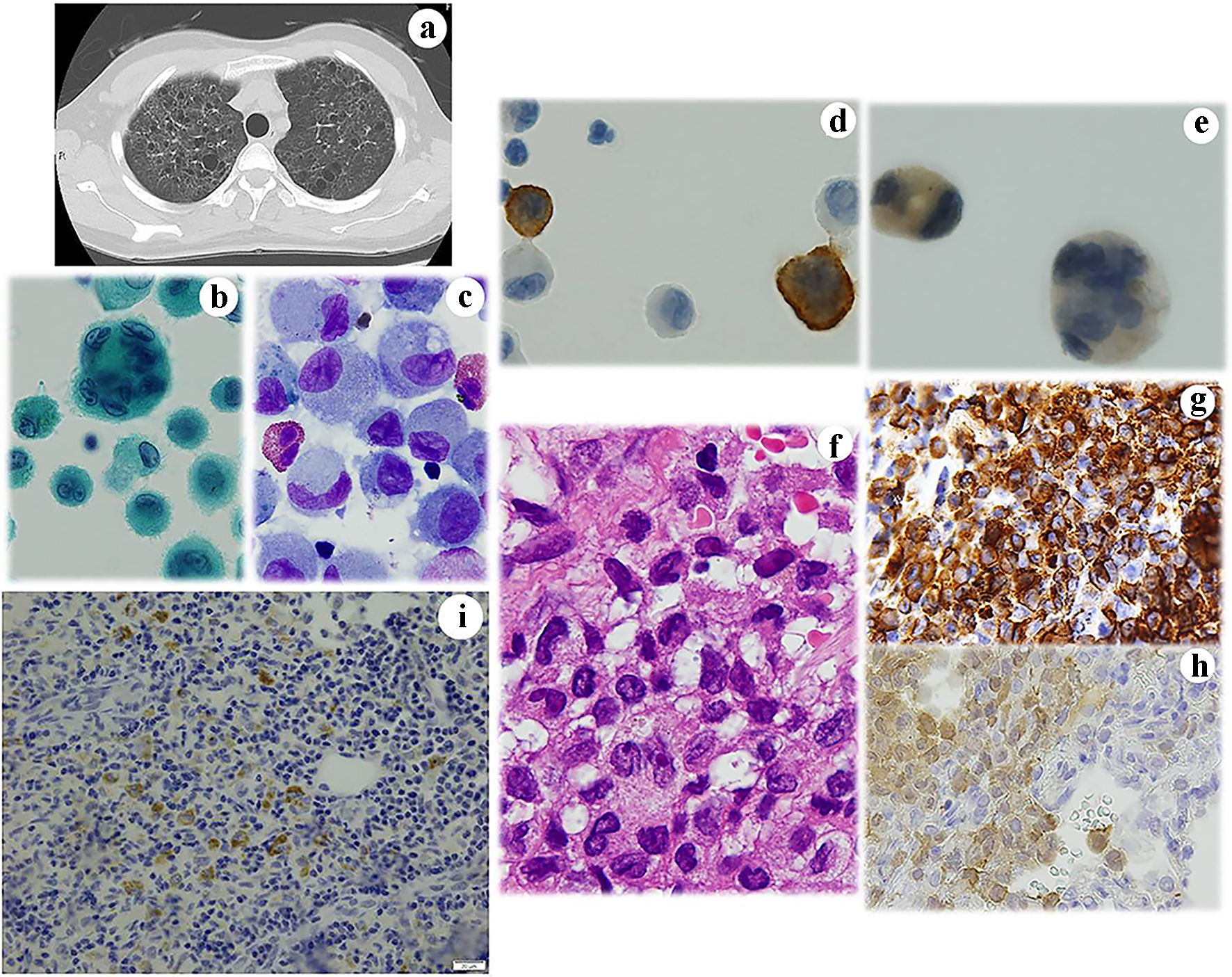
Figure 1. Case 1. (a) Chest CT shows small cystic lesions in the bilateral lungs. BALF cytology. Note the presence of large histiocyte-like cells with (b) multiple nuclei and (c) prominent grooved nuclei. These cells are immunocytochemically positive for (d) CD1a and (e) S100. Histopathologically, the lesion contains (f) abnormal histiocytes with grooved nuclei. Immunohistochemistry reveals that they are strongly positive for (g) CD1a and weakly positive for (h) S100. Some are positive for BRAFV600E antibodies. (b) Papanicolaou staining, × 400; (c) Giemsa staining, × 400; (d) CD1a immunocytochemistry; (e) S100 immunocytochemistry, × 400; (f) Hematoxylin and eosin staining, × 400; (g) CD1a immunohistochemistry, × 400; (h) S100 immunohistochemistry; and (i) BRAFV600E immunohistochemistry. CT: computed tomography; BALF: bronchoalveolar lavage fluid.
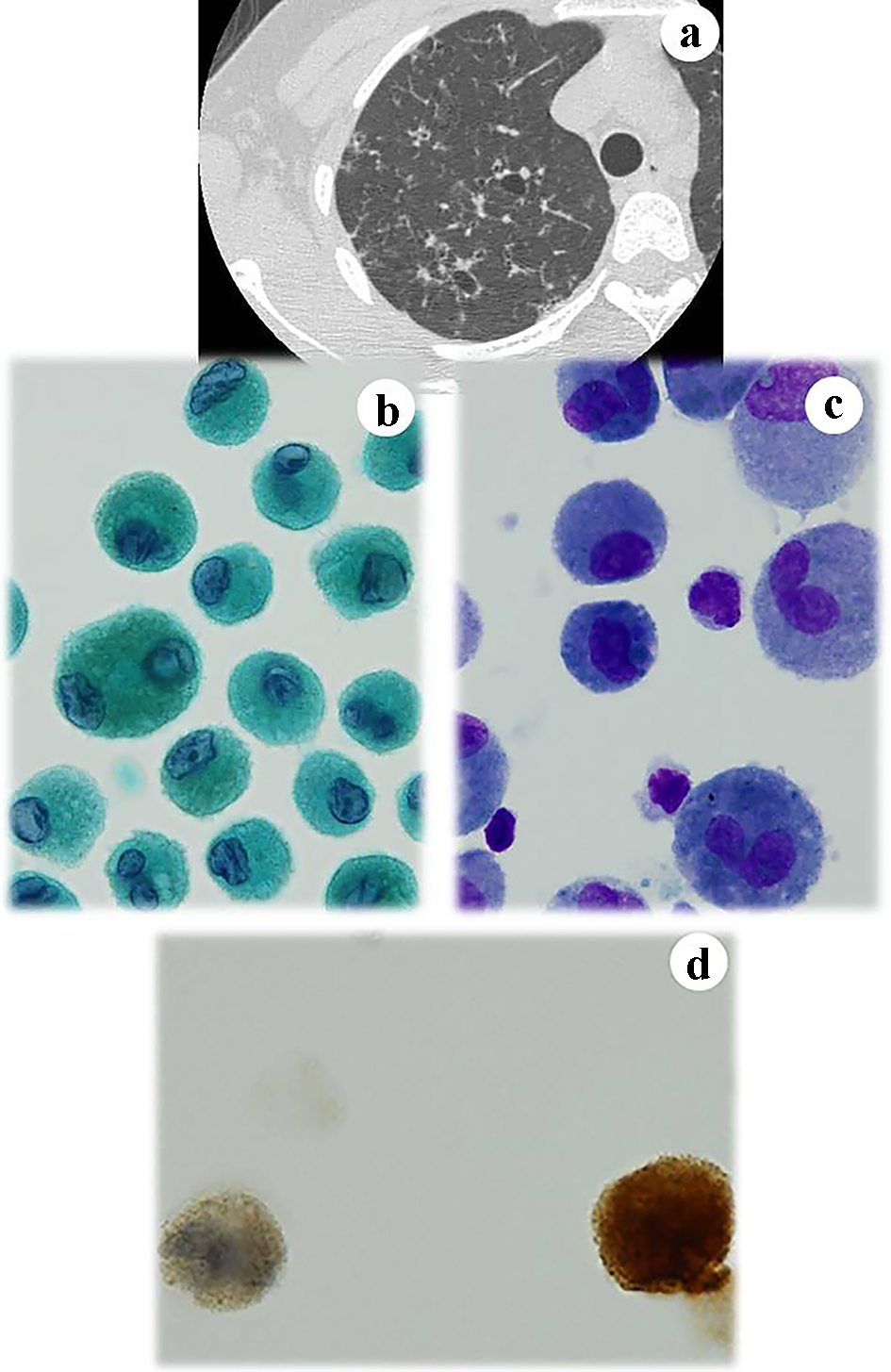
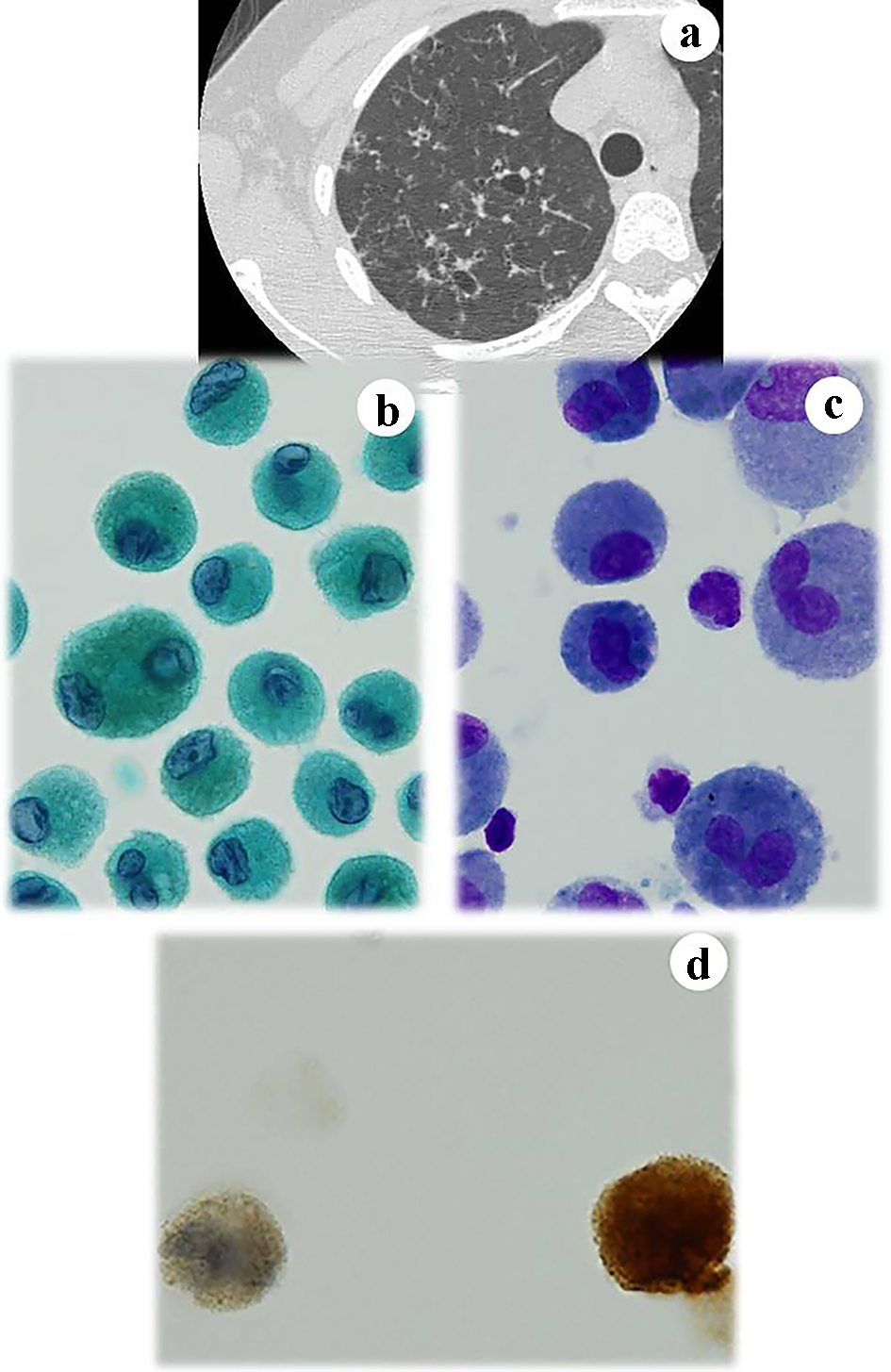
Figure 2. Case 2. CT of the lung reveals small cystic lesions in the right lung (a). A number of mononuclear and binuclear histiocytes are found in the BALF. They have (b) grooved nuclei and (c) prominent nucleoli. The cells are immunocytochemically positive for (d) S100. (b) Papanicolaou staining, × 400; (c) Giemsa staining, × 400; and (d) S100 immunocytochemistry, × 400. CT: computed tomography; BALF: bronchoalveolar lavage fluid.
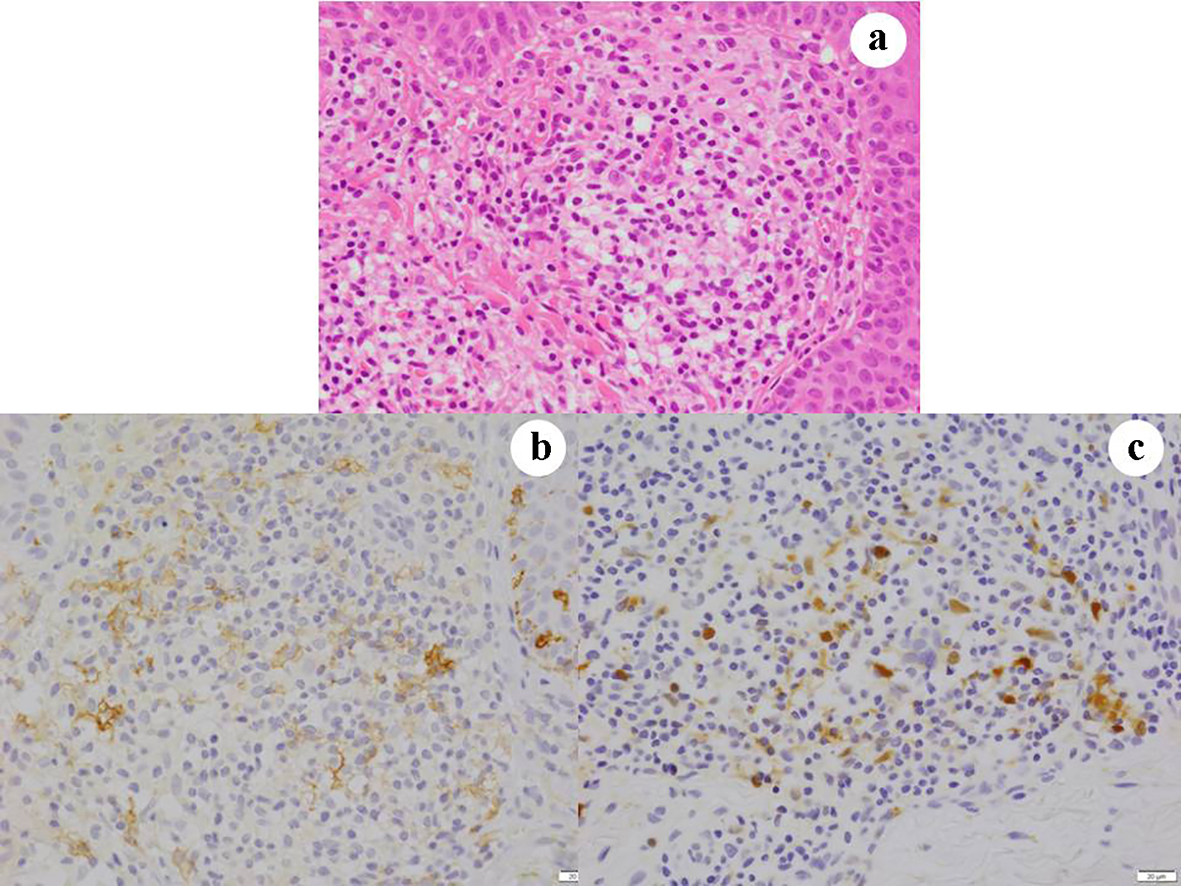
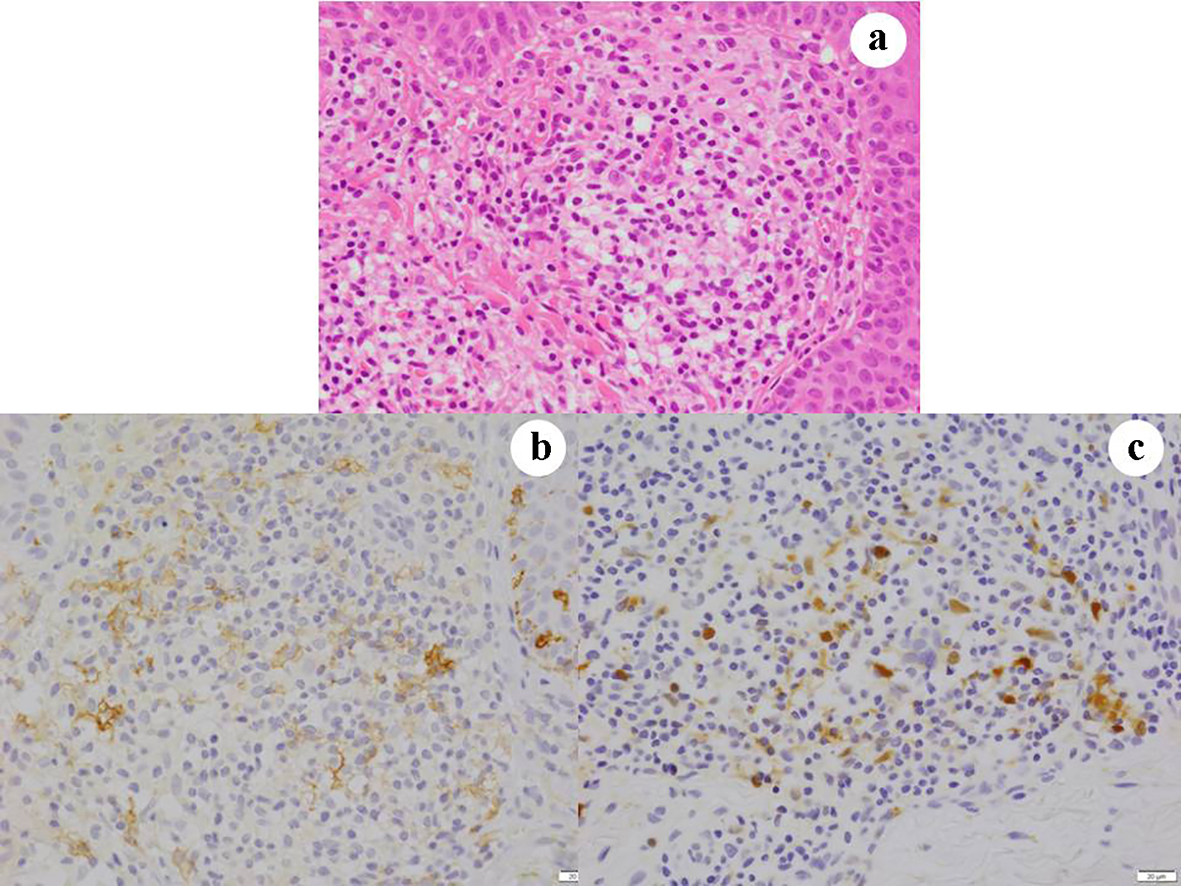
Figure 3. Case 3. Skin lesions consist of granulomatous lesions in the dermis (a). The lesions contain atypical histiocytes that are immunohistochemically positive for (b) CD1a and (c) S100. (a) Hematoxylin and eosin staining, × 400; (b) CD1a immunohistochemistry, × 400; and (c) S100 immunohistochemistry.
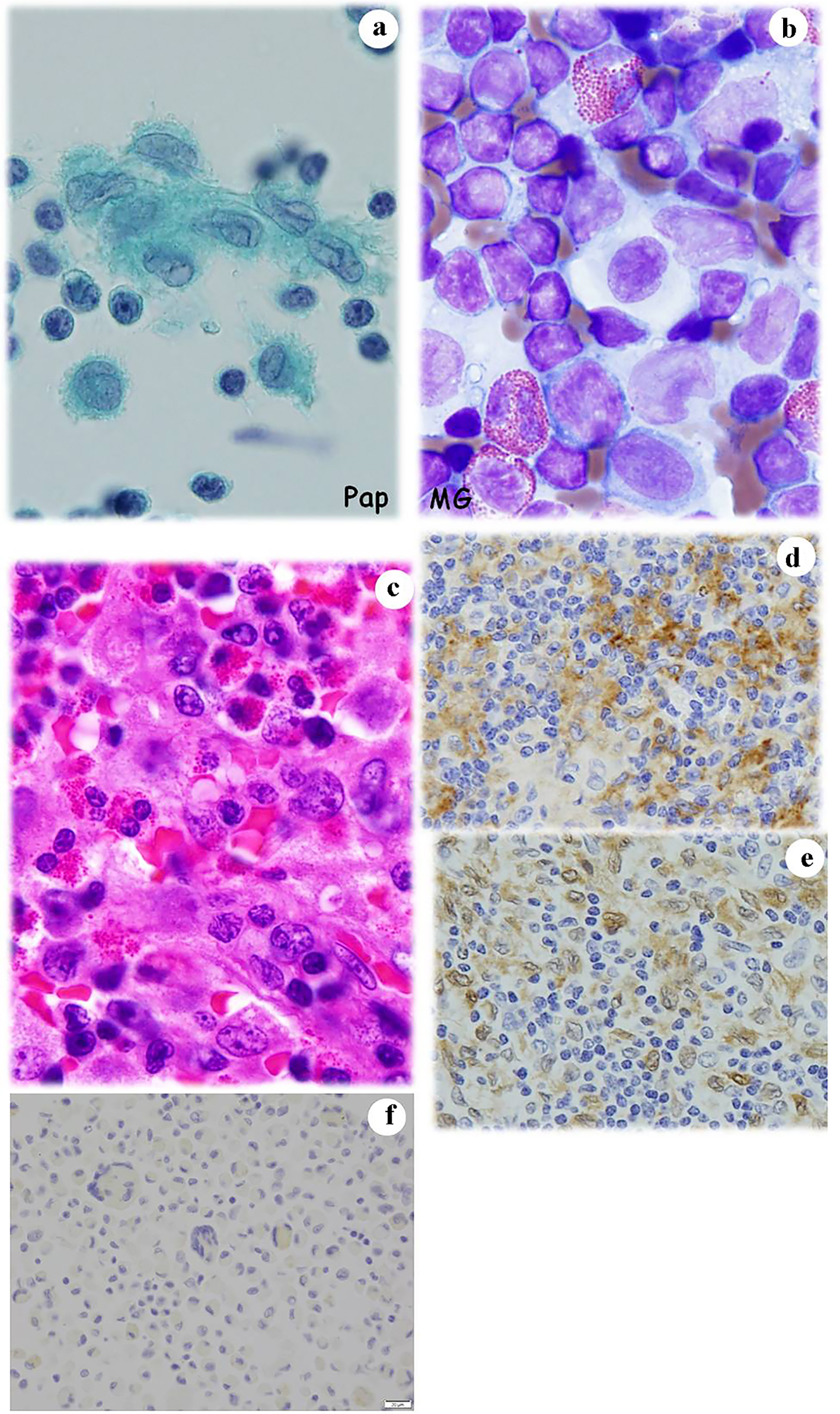
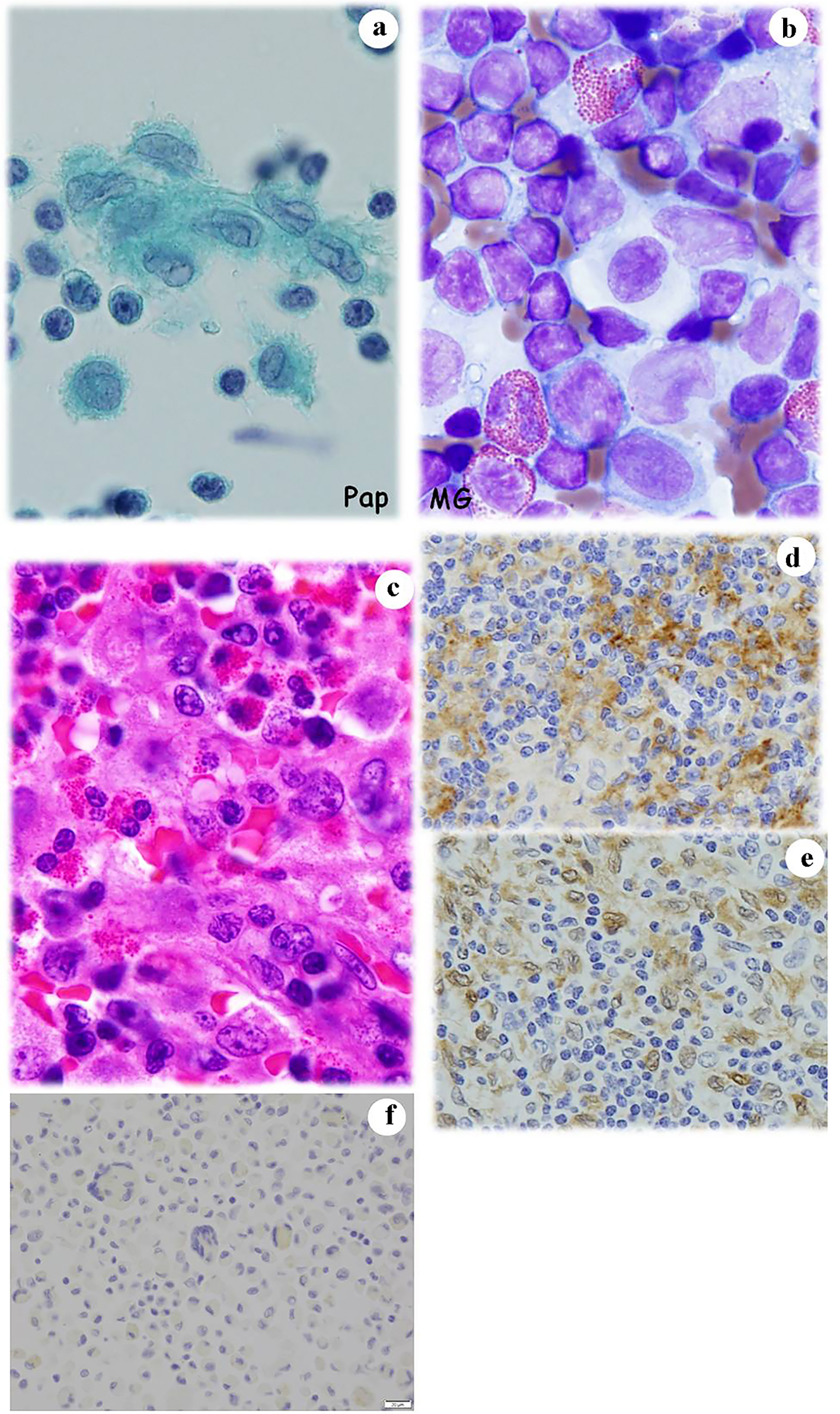
Figure 4. Case 4. Stamp cytology of enlarged lymph nodes reveals that they contain numerous large histiocytes with irregular and grooved nuclei (a) accompanied with eosinophils (b). Histopathologically, the lesions consist of atypical histiocytes and are surrounded by eosinophils (c). Immunohistochemically, atypical histiocytes are positive for (d) CD1a and (e) S100. Some of the atypical histiocytes in the lesion are weakly positive for BRAFV600E. (a) Papanicolaou staining, × 400; (b) Giemsa staining, × 400; (c) Hematoxylin and eosin staining, × 400; (d) CD1a immunohistochemistry, × 400; (e) S100 immunohistochemistry; and (f) BRAFV600E immunohistochemistry.
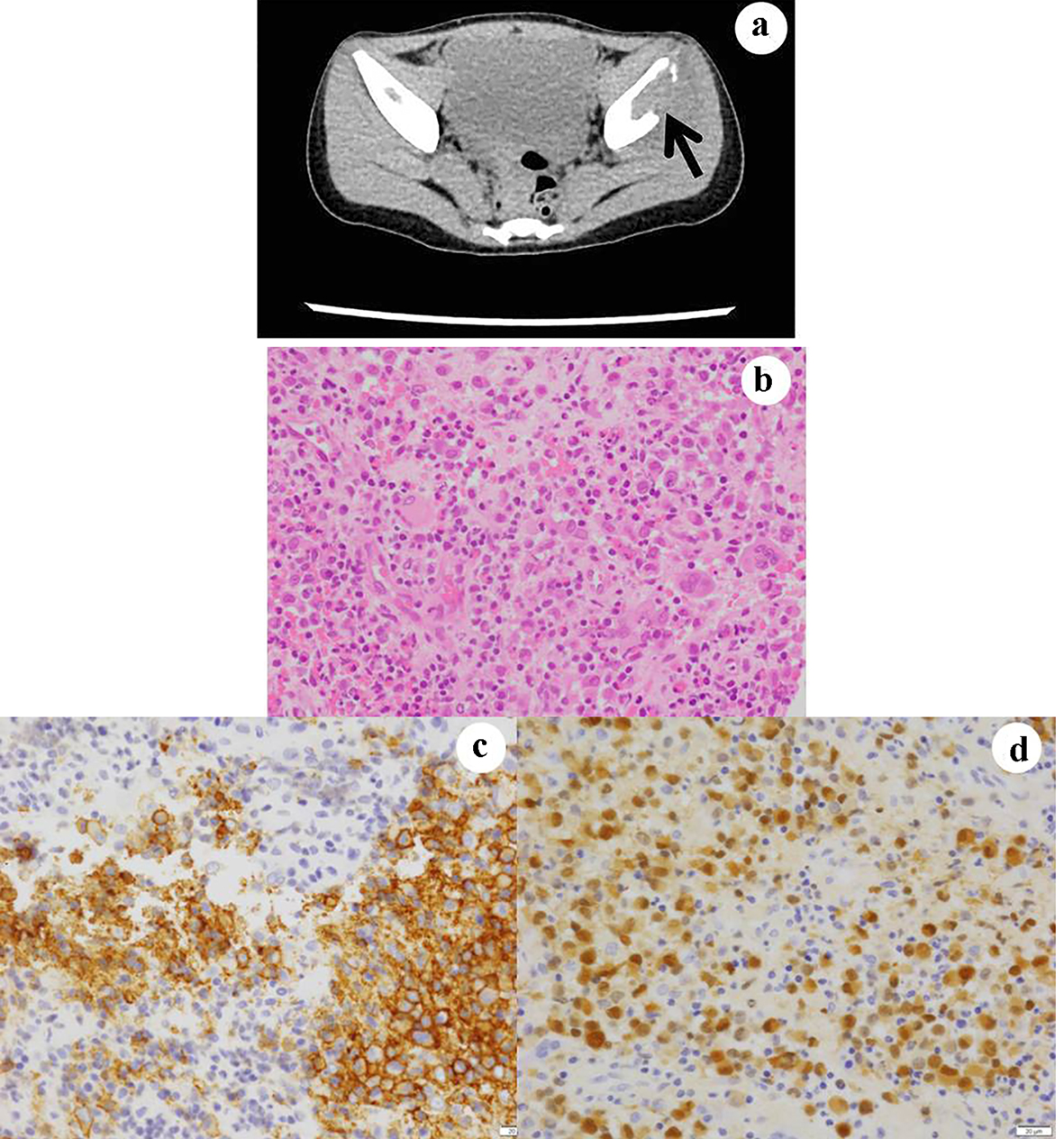
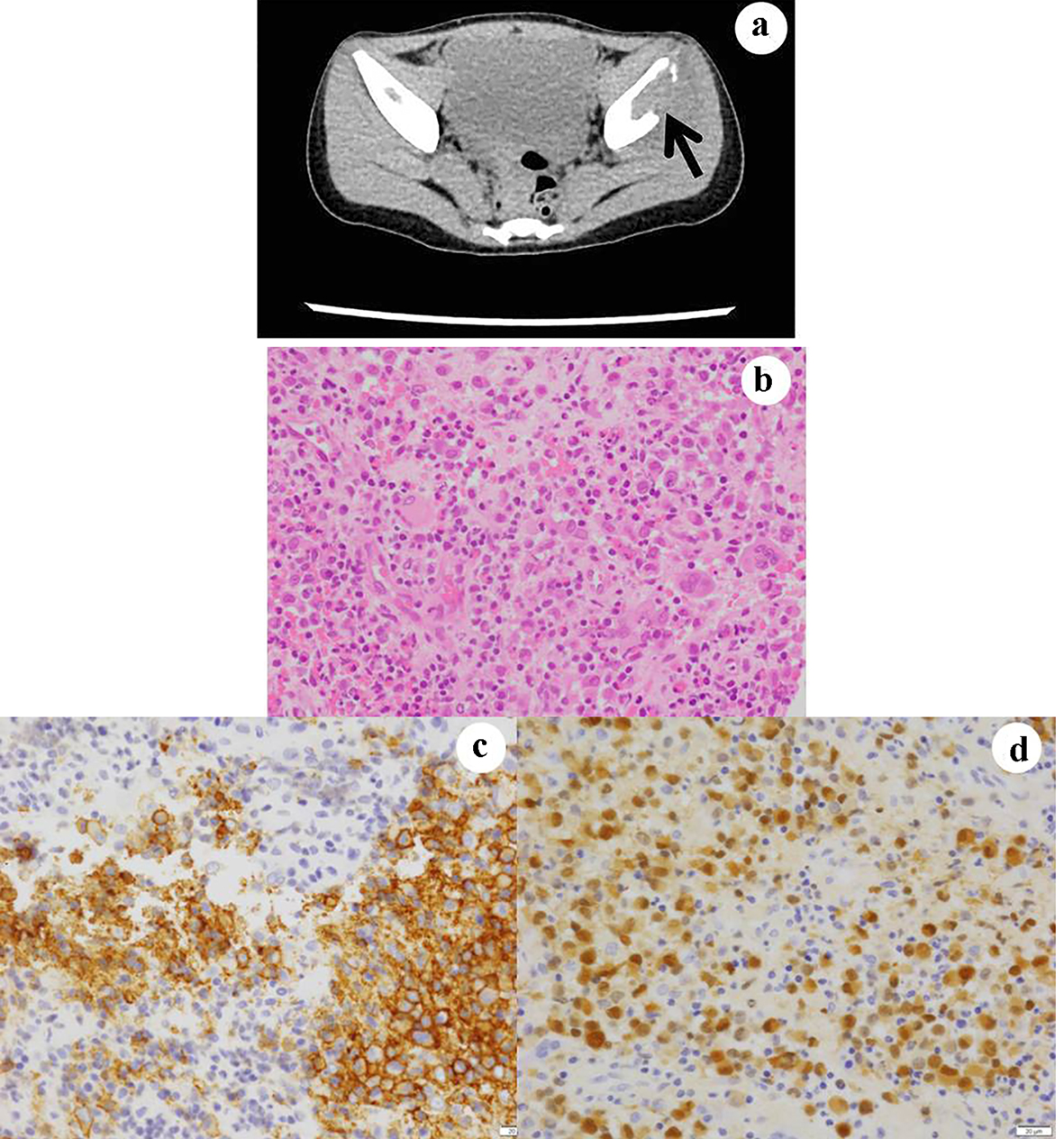
Figure 5. Case 5. The CT examination reveals osteolytic lesion in the iliac bones (a). In the biopsy specimens from the lesions, atypical and large histiocytes with single or multiple nuclei are present (b). They are immunohistochemically positive for (c) CD1a and (d) S100. (b) Hematoxylin and eosin stain, × 400; (c) CD1a immunohistochemistry, × 400; and (d) S100 immunohistochemistry. CT: computed tomography.
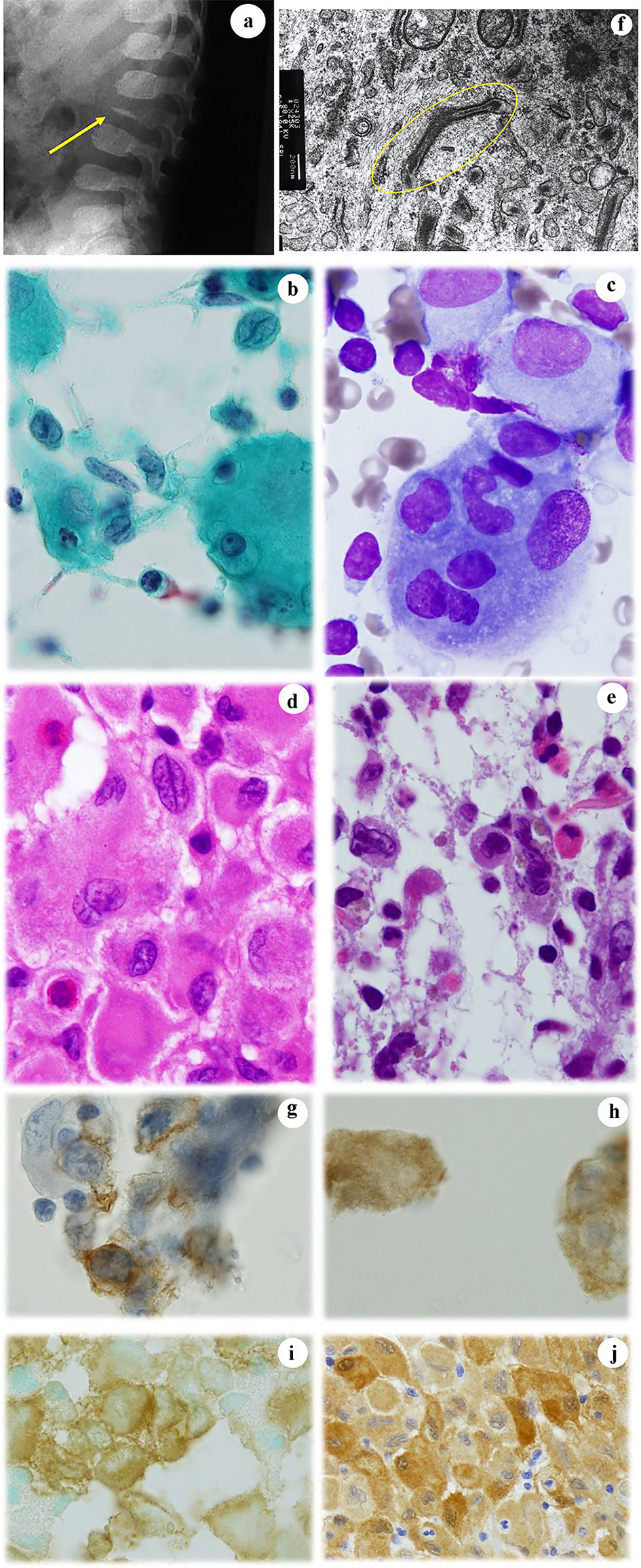
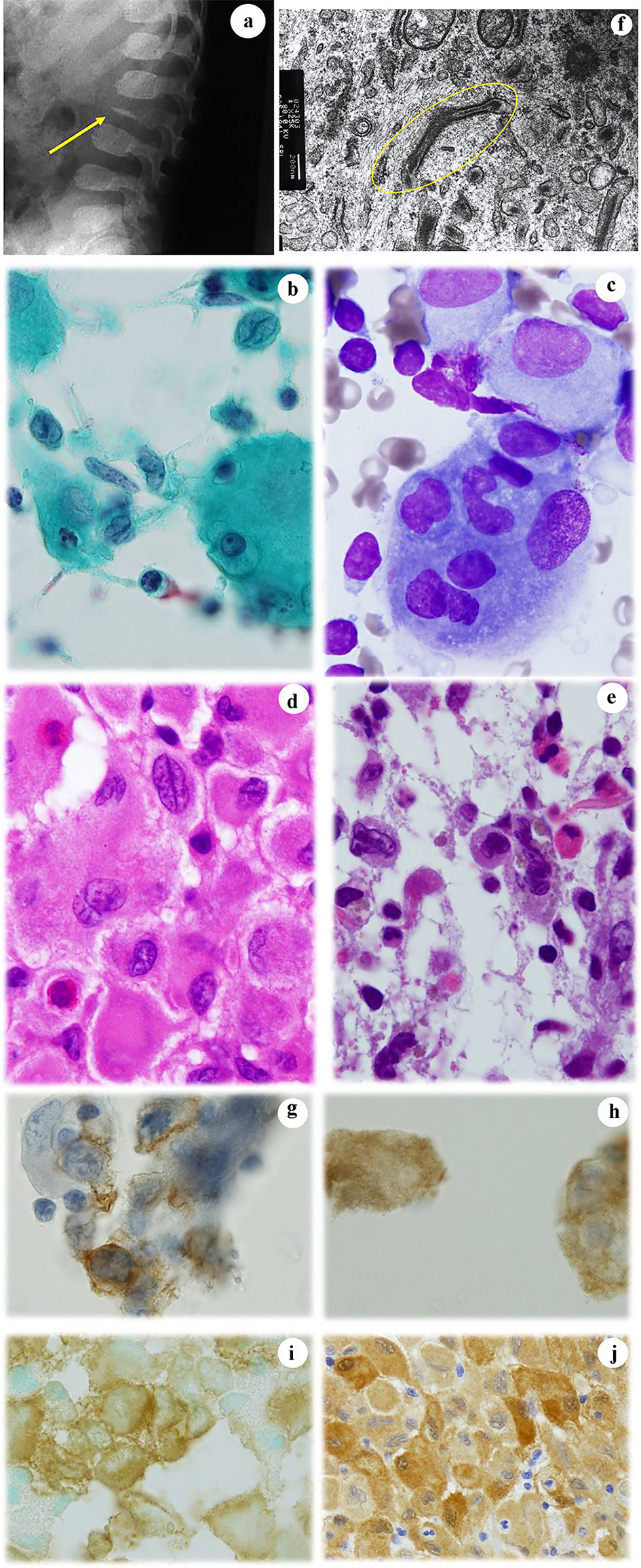
Figure 6. Case 6. (a) An X-ray examination shows platyspondyly of the lumbar calf (arrow). FNA cytology from the enlarged cervical lymph node shows a number of atypical and large histiocytes with single or multiple nuclei that have coffee bean-like grooves (b) or prominent nucleoli (c). Histopathologically, atypical and large histiocytes with grooves that are located together with eosinophils are noted in the biopsy specimens from (d) lymph node and (e) femur. EM examination reveals Birbeck’s granules (circled) in an atypical histiocyte (f). Atypical histiocytes are immunocytochemically positive for (g) CD1a and (h) S100. They are also immunohistochemically positive for (i) CD1a and (j) S100. (b) Papanicolaou staining, × 400; (c) Giemsa staining, × 400; (d) Hematoxylin and eosin staining, × 400; (e) Hematoxylin and eosin staining, × 400; (f) EM, × 62,500; (g) CD1a immunocytochemistry; (h) S100 immunocytochemistry, × 400; (i) CD1a immunohistochemistry, × 400; and (j) S100 immunohistochemistry. FNA: fine needle aspiration; EM: electron microscopy.
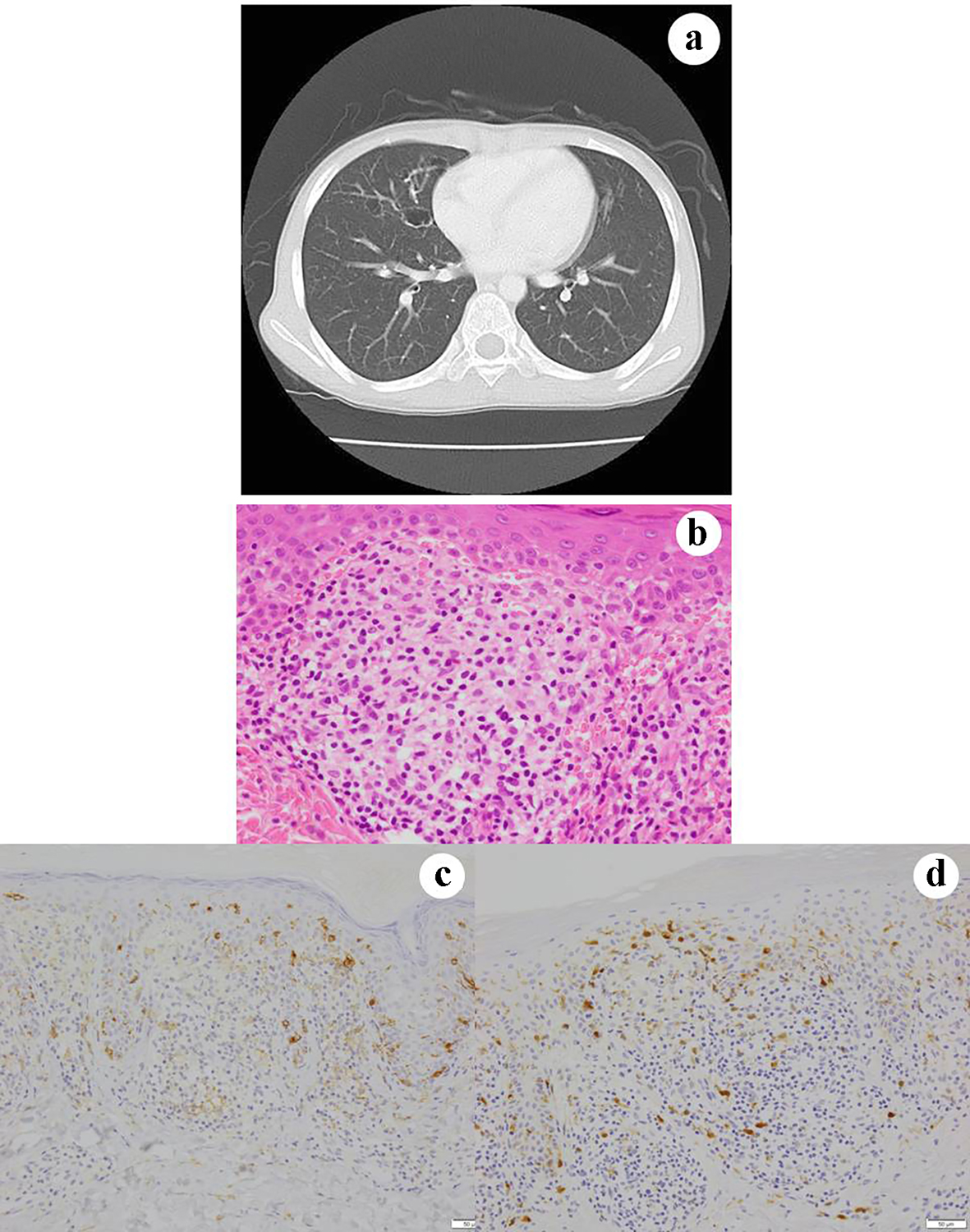
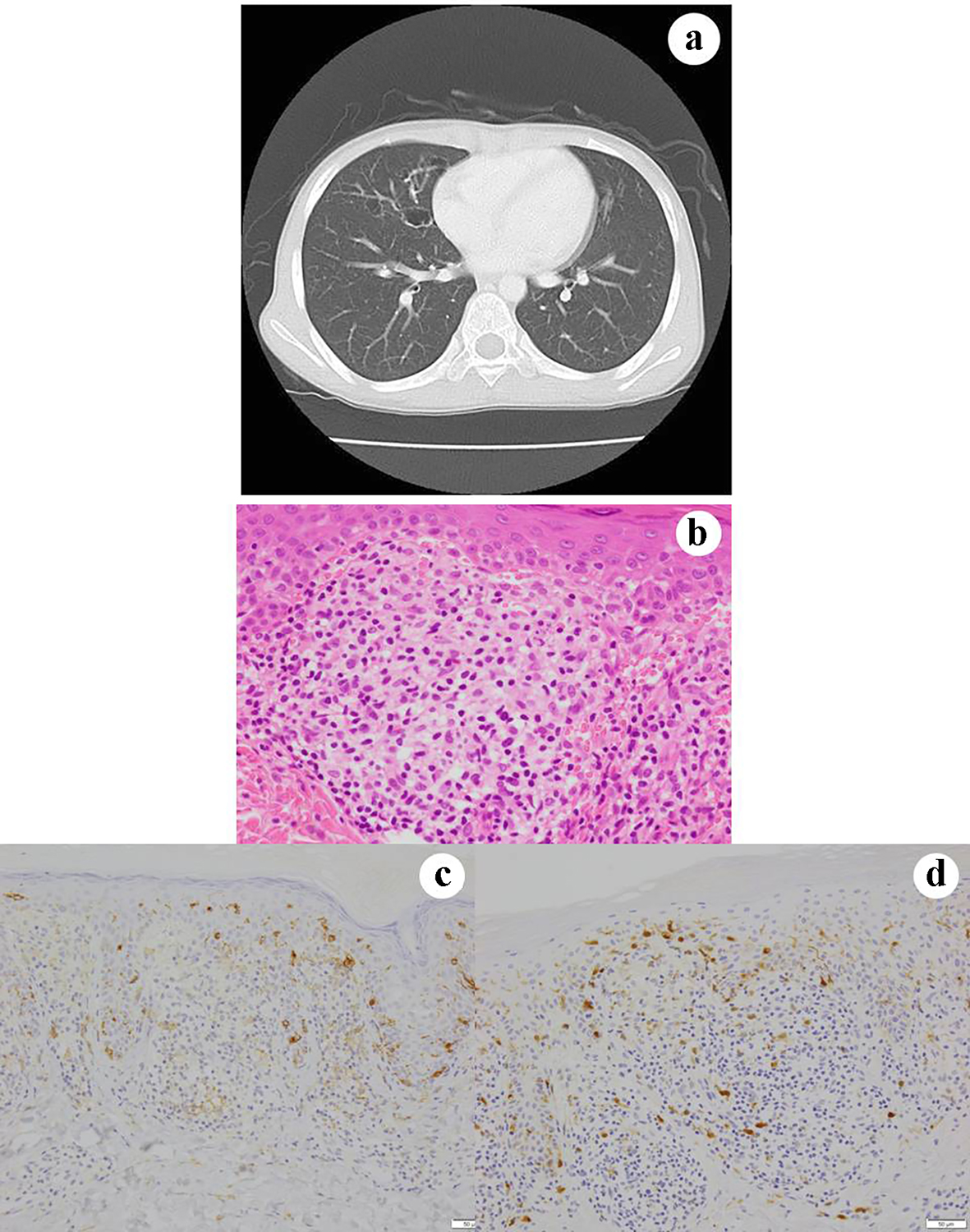
Figure 7. Case 7 (consultation case). Chest CT shows a cystic lesion in the right lung (a). Skin biopsy of the lesion shows granulomatous tissue in the dermis (b). CD1 positivity in the epidermis reveals the presence of native dendritic LCs. The lesion contains histiocyte-like cells that are weakly immunohistochemically positive for (c) CD1a and (d) S100. (b) Hematoxylin and eosin staining, × 400; (c) CD1a immunohistochemistry, × 400; and (d) S100 immunohistochemistry. CT: computed tomography; LCs: Langerhans cells.
Tables
Table 1. Clinical Classifications of LCH
| *Risk organ involvement is defined by the presence of at least one of the following: hematopoietic system (bicytopenia or pancytopenia), liver (hepatomegaly and/or dysfunction) and/or spleen (splenomegaly). LCH: Langerhans cell histiocytosis; SS-LCH: single-system LCH; MS-LCH: multisystem LCH. |
| SS-LCH: one organ/system involved (unifocal or multifocal) |
| Bone unifocal (single bone) or multifocal (> 1 bone) |
| Skin |
| Lymph node, single or multiple |
| Lung |
| Central nervous system |
| Other rare locations (e.g. thyroid, thymus) |
| MS-LCH: two or more organs/systems involved with or without the involvement of risk organs* |
Table 2. Stratification of MS-LCH
| Risk | Criteria |
|---|
| *Risk organ involvement is defined by the presence of at least one of the following: hematopoietic system (bicytopenia or pancytopenia), liver (hepatomegaly and/or dysfunction) and/or spleen (splenomegaly). MS-LCH: multisystem Langerhans ell histiocytosis. |
| Low risk | MS-LCH without the involvement of risk organs* at the diagnosis |
| High risk | MS-LCH with the involvement of risk organs at the diagnosis |
| Very high risk | High-risk patients without a response to 6 weeks of standard treatment |
Table 3. Characteristics of Seven Cases of LCH
| Case no. | Chief complaint | Age at diagnosis/gender/year of diagnosis | Initial site of involvement | Initial staging CT scans/bone marrow involvement | Recurrence | IHC and/or ICC | Therapy | Vital state |
|---|
| *Chemotherapy included vincristine (VCR)/cytarabine (Ara-C)/PSL, VCR/methotrexate (MTX)/PSL and MTX/PSL. LCH: Langerhans cell histiocytosis; F: female; M: male; IHC: immunohistochemistry; ICC: immunocytochemistry; CNS: central nervous system; PSL: prednisolone. |
| 1 | Chest pain | 35/F/2016 | Lung/rib | Yes/no | No | S100, CD1a | Smoking cessation | Alive |
| 2 | Medical examination | 28/F/2017 | Lung | Yes/no | No | CD1a | Smoking cessation | Alive |
| 3 | Erythema | 33/M/2014 | Skin | Yes/no | No | S100, CD1a, CD45RO | PSL | Alive |
| 4 | Erythroderma | 58/M/2008 | Lymph nodes (inguinal) | Yes/no | No | S100, CD1a | PSL | Alive |
| 5 | Claudication | 2/F/2014 | Ilium/skull | Yes/yes | No | S100, CD1a | PSL and chemotherapy* | Alive |
| 6 | Fever | 1/F/2005 | Femur/skull/vertebral body/lymph nodes (cervical and abdominal) | Yes/yes | No | S100, CD1a, CD68 | PSL and chemotherapy | Alive |
| 7 | Polydipsia urine | 9/F/2010 | Skin/lung/CNS/lymph node (cervical) | Yes/yes | No | S100, CD1a | Chemotherapy | Alive |