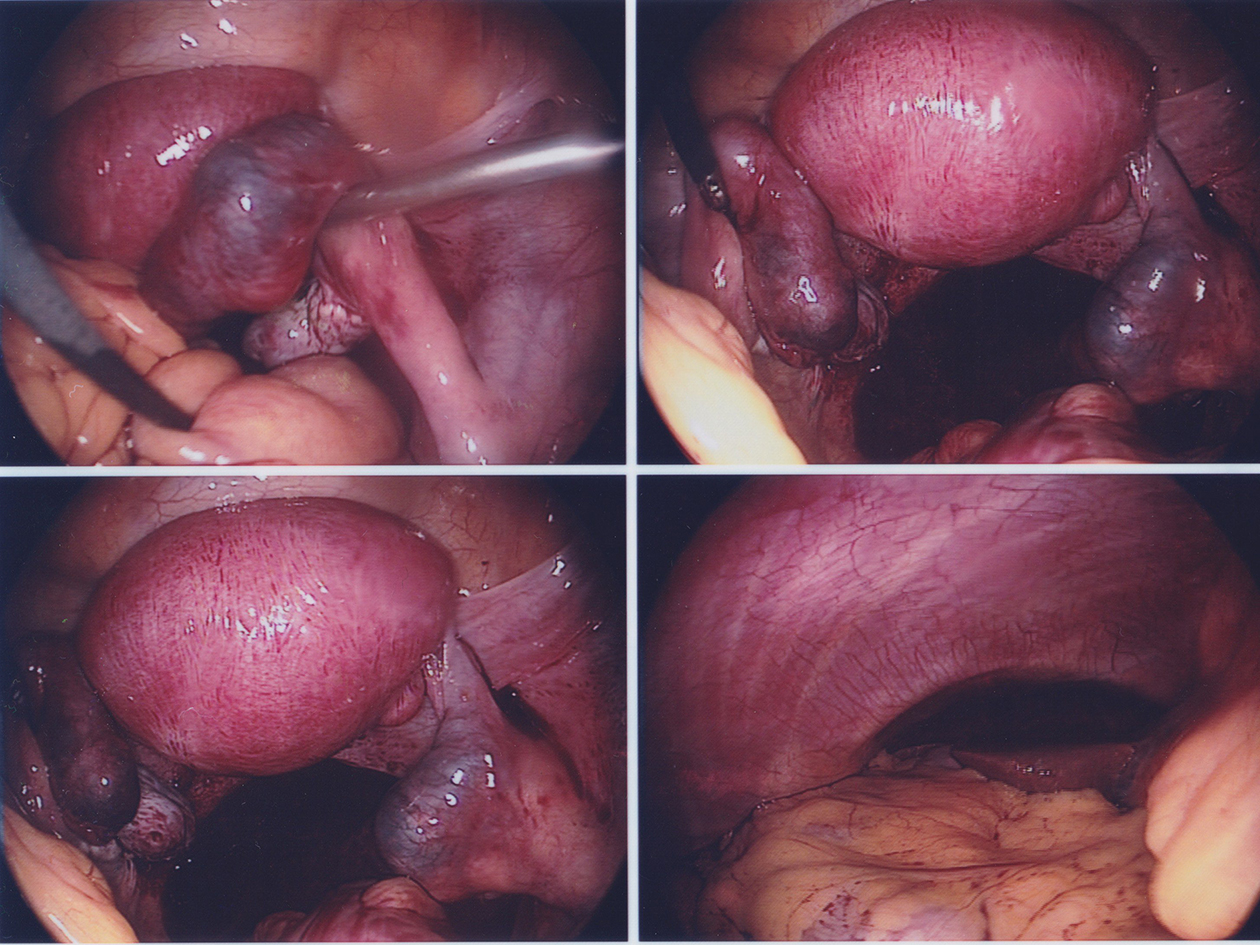
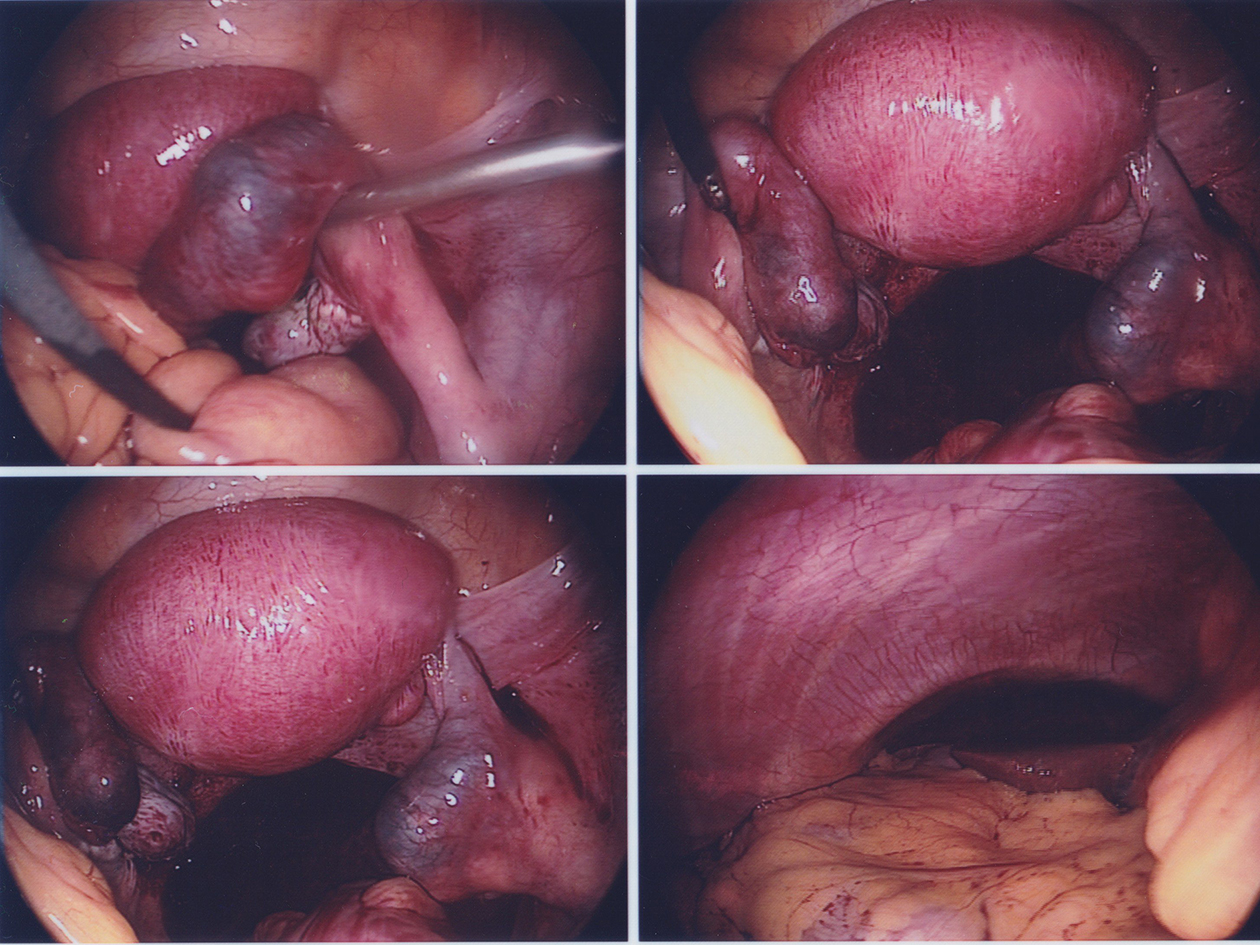
Figure 1. (Clockwise from top right) Right ectopic pregnancy; left tube with phimosed end likely ectopic pregnancy; hemoperitoneum from ruptured right ectopic pregnancy; view of the normal liver.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 7, July 2016, pages 286-290
A Case of Bilateral Ectopic Pregnancy Following Intra-Uterine Insemination
Figure
Tables
| Date | 29/12/2014 | 3/1/2015 | 5/1/2015 | 9/1/2015 | 15/1/2015 |
|---|---|---|---|---|---|
| Symptoms/events | Day 17 after IUI | Presented with vaginal spotting (day 22 after IUI) | 48 h after first b-hCG (trending) | Day 4 after methotrexate administration | Returned to emergency unit with clinical features of acute abdomen. Day 10 after methotrexate |
| b-hCG (IU/L) | 273.3 | 2,858 | 4,123.2 | 6,847.5 | 1,651.8 |
| Ultrasound findings | No IUGS seen | 1.3 × 0.7 × 0.7 cm ring-like structure in right adnexa with yolk sac. No free fluid | 1.3 × 1.3 × 1.1 cm ring-like structure in right adnexa with yolk sac. No free fluid | Free fluid in pelvis Right adnexal mass 1.7 × 1.7 cm | |
| Management options | Options of conservative/surgery and methotrexate offered. Patient keen for methotrexate | Option of diagnostic laparoscopy offered with the view of salpingostomy or salpingectomy | Option of diagnostic laparoscopy offered in view of hemoperitoneum from ruptured ectopic pregnancy | ||
| Summary of management plan | IM methotrexate 90 mg administered | Patient declined intervention | Proceeded with diagnostic laparoscopy |
| Title | Investigation/diagnosis | Management | Conclusion |
|---|---|---|---|
| A rare case of bilateral ectopic pregnancy and differential diagnosis of gestational trophoblastic disease [1] | Initial high titres of B-hCG with a negative diagnostic evacuation of uterus done for suspicion of GTD. Repeated ultrasound found unilateral ectopic pregnancy. | Laparotomy with findings of bilateral ampullary pregnancies. Bilateral salpingostomies done and methotrexate administered post-operatively. | Laparotomy with findings of bilateral ampullary pregnancies. Bilateral salpingostomies done and methotrexate administered post-operatively. |
| Heterochronic bilateral ectopic pregnancy after ovulation induction [2] | Patient presented with symptoms of per vaginal bleeding and right abdominal pain. TV ultrasound showed right adnexal mass suggestive of 4 cm right ampullary ectopic pregnancy. | Laparoscopy showed 4 cm unruptured right ampullary ectopic pregnancy and was histologically confirmed. Left fallopian tube was inspected and deemed normal. B-hCG rose after post-operative decrease. TV ultrasound 21 days later showed left adnexa mass 2.2 cm. IM methotrexate administrated. Three days later patient presented with hemoperitoneum. Laparoscopy confirmed a left ectopic pregnancy and a left salpingectomy was performed. | Because of the difficulty in identification of bilateral ectopic pregnancy by ultrasonography, the clinician should be aware that the treatment of one ectopic pregnancy does not preclude the occurrence of a second ectopic pregnancy in the same patient and should pay attention to the intra-operation inspection of both side fallopian tubes in any ectopic pregnancy case. |
| Bilateral ectopic pregnancy following ICSI [3] | Ultrasound failed to show IUGS despite normal and reassuring B-hCG trend. | Laparoscopic salpingostomy for one side and salpingectomy for the other side. | Bilateral tubal ectopic pregnancy is a rare clinical condition. Following surgical management of this condition, it is still possible to conceive with future ICSI-ET attempts. |
| Bilateral tubal ectopic pregnancy following intra-uterine insemination (IUI): a case report [4] | Patient presented with pain and per vaginal bleeding after IUI. Pelvic ultrasound diagnosed bilateral ectopic pregnancies with free fluid in pouch of Douglas. | Exploratory laparotomy, left salpingectomy and right salpingostomy. | Cases presenting with infertility and ectopic pregnancy should be followed very closely with B-hCG and/or transvaginal sonography (TVS) to exclude double ectopic. |
| A case of bilateral tubal pregnancy after IVF-ET [5] (article in Bulgarian) | Post ET on day 36 patient presented with abdominal pain in right hypogastrium. | Urgent laparotomy performed with salpingectomy due to hemoperitoneum from tubal rupture on one side. Decision undertaken for left salpingectomy after visual diagnosis of left unruptured tubal pregnancy. Histology confirmed bilateral ectopic pregnancies. | The frequency of some rare forms and locations of ectopic as well as heterotopic pregnancies increase after ART. |
| Bilateral ampullary pregnancy after clomifen-citrate and intrauterine insemination - a unique case report [6] | After clomiphene and IUI, patient presented with right abdominal pain with B-hCG 9,000 IU/L. Pelvic ultrasound showed a right adnexal mass 22 mm. | Laparoscopy for right tubal ectopic pregnancy with right salpingectomy performed. Left tube was inspected and deemed normal. Patient presented with left abdominal pain after surgery. Pelvic ultrasound revealed a left adnexal mass 17 mm. B-hCG was 14,000 IU/L. Repeat laparoscopy done showed left ectopic pregnancy with left salpingectomy done. Histology confirmed bilateral ectopic pregnancies. | Clomifen-citrate induced cycle might result in bilateral heterotopic pregnancy not only after insemination, but also after intercourse. This condition must always be considered in emergency situations. |
| Bilateral simultaneous isthmic ectopic pregnancy after clomiphene induction [7] | After clomiphene and IUI, patient presented with light vaginal bleeding and mild abdominal pain. | In cases of ectopic pregnancy with ovulation induced by clomiphene citrate, doctors must be aware of the possibility of bilaterality. | |
| A case report of bilateral tubal ectopic pregnancy following day 5 embryo transfer [8] | Patient presented with vaginal bleeding and abdominal pain after ICSI. Ultrasound showed 23 mm left adnexal mass suggestive of ectopic pregnancy. | Laparoscopy showed 3 cm unruptured left ampullary ectopic pregnancy. Salpingostomy performed. Inspection of right tube showed bulging area in ampullary region. Salpingostomy was done. Histology confirmed placental villi in right and left tubes. | When a diagnosis of ectopic pregnancy is made, both adnexa should be examined in order to prevent maternal morbidity and mortality. Reducing the number of transferred embryos can lessen bilateral tubal pregnancies. |
| Simultaneous bilateral tubal pregnancy after in vitro fertilization and embryo transfer [9] | Patient presented 32 days after ET for pelvic pain and vaginal bleeding. TV ultrasound revealed a live ectopic pregnancy in the right fallopian tube as well as a left ectopic pregnancy. B-hCG was 3,091 IU/L. | Laparoscopy confirmed ultrasound findings. Bilateral salpingostomy was performed. Histology confirmed chorionic villi and placental tissue in both tubes. | Although the incidence of bilateral tubal pregnancy is not high, sonographers and surgeons should examine both adnexa when diagnosing an ectopic pregnancy, especially in IVF-ET patients. Early diagnosis is essential for the prevention of significant maternal morbidity and mortality. |
| Combined bilateral ectopic and intrauterine pregnancy following ovulation induction with the low-dose step-up protocol in a patient with polycystic ovary syndrome [10] | Patient initially presented with a spontaneous miscarriage, and transvaginal ultrasonography revealed an empty uterus. However, 4 days later, the patient presented with an acute abdomen. Laparoscopy revealed bilateral tubal pregnancy with hemoperitoneum. The right tubal pregnancy was intact and the left one was ruptured with extensive tubal damage. | After a spontaneous miscarriage she was treated by laparoscopic left salpingectomy and right linear salpingotomy. | A woman with polycystic ovary syndrome (PCOS) developed bilateral tubal and an intrauterine pregnancy following ovulation induction with urinary FSH using the low-dose step-up protocol. |