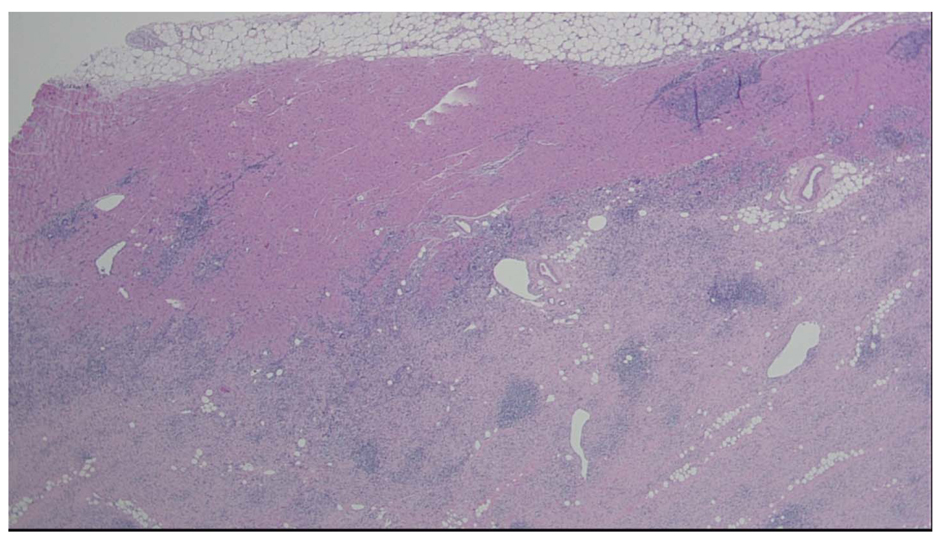
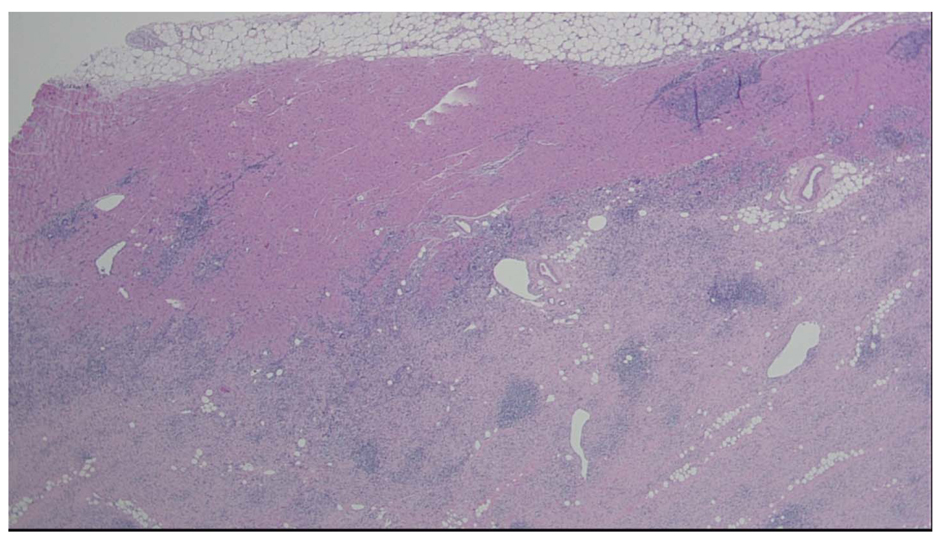
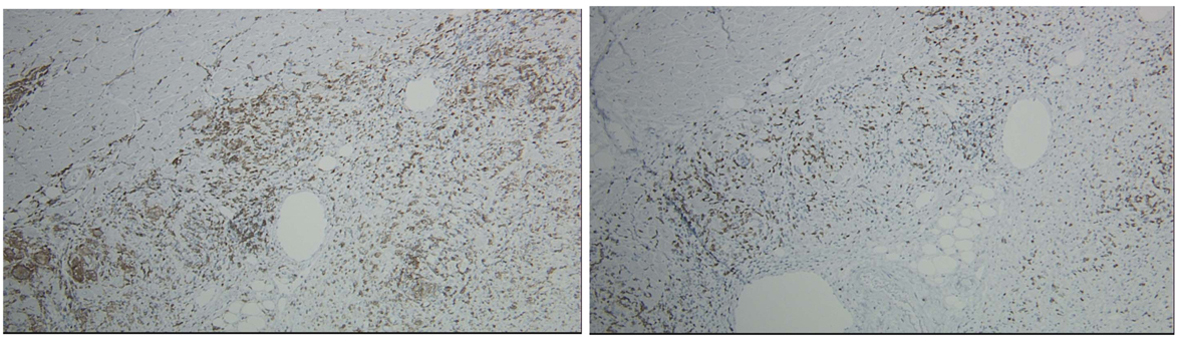
Figure 1. Heart, apical core biopsy. Section of myocardial biopsy shows extensive myocardial necrosis and chronic inflammation with lymphocytes, eosinophils, and many giant cells. No granulomas are identified. Giant Cell Myocarditis 4 × H & E Stain
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 12, December 2013, pages 775-779
Infiltrative Disease in Non-Ischemic Cardiomyopathy: Giant Cell Myocarditis Leading to Fulminant Myocarditis
Figures
Tables
| Parameters Considered | Fulminant | Acute | Chronic active | Chronic persistent |
|---|---|---|---|---|
| DCM, dilated cardiomyopathy; LV, left ventricle; Permission obtained from Elsevier Ltd@ Lieberman EB et al (1991) J Am Coll Cardiol 18: 1617 – 1626. | ||||
| Onset of cardiac symptoms | Abrupt | Insidious | Insidious | Insidious |
| Initial presentation | Cardiogenic shock | Heart failure with LV dysfunction | Heart failure with LV dysfunction | Asymptomatic and no LV dysfunction |
| Initial endomyocardial biopsy findings | Multiple foci of active myocarditis | Active or borderline myocarditis | Active or borderline myocarditis | Active or borderline myocarditis |
| Clinical course | Complete recovery or death | Incomplete recovery or chronic, stable DCM | Progressive end-stage DM | Mild symptoms with stable LV function |
| Histologic course | Complete resolution | Complete resolution | Ongoing or resolving myocarditis; fibrosis and giant cells | Persistent inflammation with foci of myocyte necrosis |
| Response to immunosuppressive therapy | No benefit | Variable | Initial response followed by relapses | No benefit |
| Differential diagnosis | Associated conditions | Key clinical features | Key histologic findings | Treatment |
|---|---|---|---|---|
| Sachin G, Markham DW, Drazner MH, Mammen PP. Fulminant Myocarditis. Nat Clin Prac. 2008; 5: 693-706. | ||||
| Giant cell myocarditis | Autoimmune disorders Thymoma Drug hypersensitivity to minocycline, cephalosporins, phenytoin, primidone | Malignant ventricular tachycardia Heart block | Multinucleated giant cells | High-dose steroids and cyclosporine or azathioprine Cardiac transplantation |
| Necrotizing eosinophilic myocarditis | Allergic diathesis Churg-Strauss syndrome Idiopathic hypereosinophilic syndrome Endomyocardial fibrosis | Flu-like symptoms Peripheral blood eosinophilia | Diffuse infiltration with eosinophils and extensive myocyte necrosis | High-dose steroids |
| Sarcoidosis | Autoimmune disorders | Arrhythmias Hilar adenopathy | Noncaseating granulomas | High-dose steroids Cardiac transplantation |
| Peripartum cardiomyopathy | None | Time of onset related to pregnancy | Mild-to-moderate lymphocytic infiltration with myocyte necrosis | Spontaneous recovery High-dose steroids and azathioprine LVAD Cardiac Transplantation Bromocriptine |
| Acute myocardial infarction | Hypertension Diabetes mellitus Peripheral vascular disease Dyslipidemia | Electrocardiographic evidence of ischemia | Thrombus in coronary arteries with myocyte necrosis | Coronary angioplasty IABP LVAD |