| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 1, February 2012, pages 73-75
Primary Malignant Melanoma of the Female Urethra
Cvjetko Leza, Silvio Altaracb, Samer El-Safadic, h, Rajko Furesd, Hrvoje Cupice, Zoran Persecf, Zlatko Hrgovicg
aDepartment of Pathology and Cytology, General Hospital Zabok, Zabok, Croatia
bDepartment of Urology, General Hospital Zabok, Zabok, Croatia
cDepartment of Gynecology and Obstetrics, Universitiy Hospital Giessen and Marburg GmbH, Giessen, Germany
dDepartment of Obstetrics and Gynecology, General Hospital Zabok, Zabok, Croatia
eUniversity Department of Pathology Ljudevit Jurak, Sestre milosrdnice, University Hospital, Zagreb, Croatia
fDepartment of Urology, University Hospital Dubrava, Zagreb, Croatia
gDepartment of Gynecology and Obstetrics, Johann Wolfgang Goethe University, Frankfurt/M, Germany
hCorrespondence author: Samer El-Safadi, Klinikstr, 33, D-35392 Giessen, Germany
Manuscript accepted for publication December 7, 2011
Short title: Melanoma of Female Urethra
doi: https://doi.org/10.4021/jmc460w
| Abstract | ▴Top |
Primary malignant melanoma of the female urethra is a rare tumour that most commonly affects meatus and the distal urethra. The prognosis is poor. We report the case of 65-year-old woman which was referred by a gynaecologist due to a urethral mass mimicking a caruncule. The tumour was removed by a local excision, and pathological analysis revealed malignant melanoma. After three months distal urethrectomy was performed with no evidence of residual tumour. The patient was uneventful during 6-year follow up period.
Keywords: Female urethra; Malignant melanoma; Long term survived
| Introduction | ▴Top |
The most frequent locations of primary malignant melanoma are the skin and eye, while malignant melanoma of the lower female genitourinary tract is an uncommon malignancy [1, 2]. The urethra is the most common site of origin in primary malignant melanoma of the genitourinary tract. Most malignant melanomas of the female urethra are located at the meatus or in the distal urethra. Urethral melanoma shows its peak incidence in the older age group, the average patient aged 63 years. The disease is three times more common in women than men [3].
Reed reported the first case of primary malignant melanoma of the female urethra in 1896 [4]. The tumour is usually pigmented, varying in colour from black to blue or light brownish lesions, which are firm, nodular and often ulcerated. Grossly, the tumour may be easily confused with a caruncule [5]. Primary malignant melanoma of the female urethra tends to metastasize at the early stage via the superficial lymphatics to the vulva and vagina, by the deep lymphatics to the inguinal lymph nodes and occasionally to distant sites by the haematogenous route. Survival depends on the stage, location and size of the neoplasm at the time of diagnosis. Histological characteristics do not affect the prognosis significantly and all histological types are treated in a similar manner [3, 6]. Despite major surgery, radiotherapy or immunotherapy malignant melanoma usually has a poor prognosis[7]. Most patients do not survive more than three years. Only eleven patients so far have been reported who lived for 4 years and more [7-10]. We report an additional case of patient who is alive and well after 6 year.
| Case Report | ▴Top |
A 65-year-old woman was referred by a gynaecologist due to a urethral mass with a gross appearance of a caruncule. Upon examination a 3 cm wide pedunculated black pigmented friable and hemorrhagic polyp was found at the posterior wall of the urethral meatus. The tumour was removed by a local excision. Histopathologic analysis revealed polypoid tumour with surface partially ulcerated and partially covered with squamous and transitional epithelia (Fig. 1). The tumour is composed of loosely cohesive nests of atypical epiteheloid and spindle shaped melanocytes showing diffuse and nested growth pattern. The neoplastic cells had abundant eosinophilic cytoplasm, large hyperchromatic nuclei with prominent nucleoli and brisk mitotic activity (15/10 HPF). Most of the tumour cells contained coarsely granular melanocytic pigment (Fig. 2). Depth of tumour invasion, measured by digital microscopic camera Olympus DP10 is 3.57 mm. No vascular/lymphatic invasion was seen histologically. Immunohistochemically tumour cells showed strong cytoplasmatic reactivity for HMB-45 and S100 (Fig. 3). The low third resection of distal urethra was performed in another institution three months after initial surgery with no evidence of residual tumour. Initial metastatic evaluation including computerized tomography scan of the chest, abdomen and pelvis revealed no evidence of disseminated disease. Computerized tomography after two years after initial diagnosis revealed two enlarged right parailiacal lymph nodes which remained unchanged at two subsequent CT controls performed four and six years later. The patient was uneventful during 6-year follow-up period.
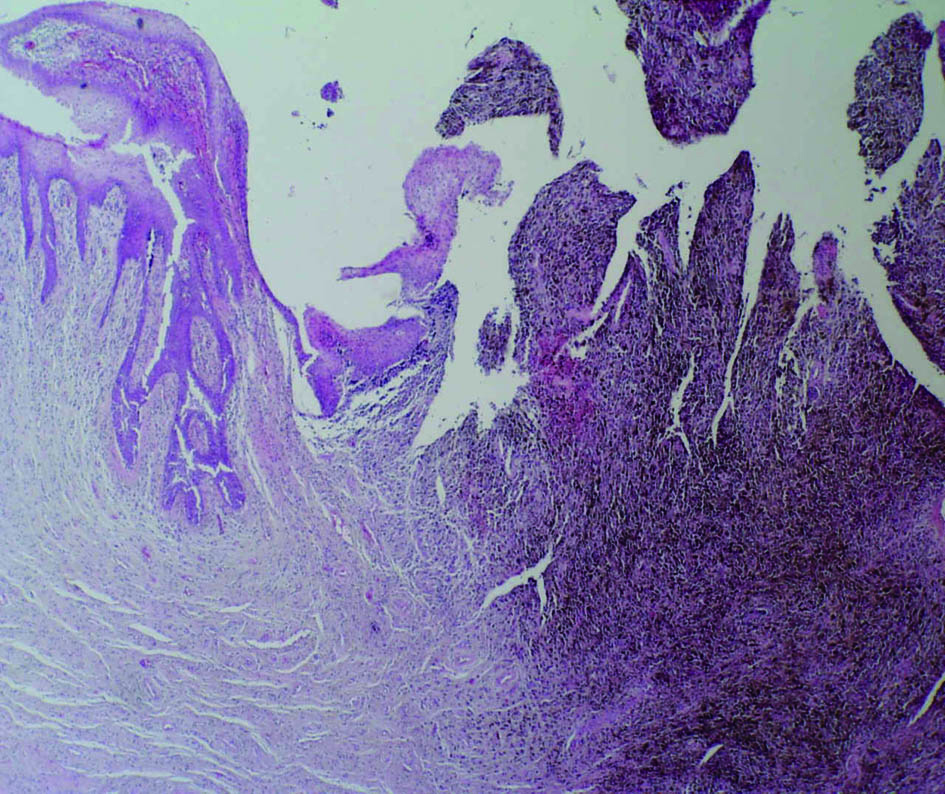 Click for large image | Figure 1. Polypoid, partially ulcerated melanoma of the female urethra (hematoxylin and eosin stain ×40) |
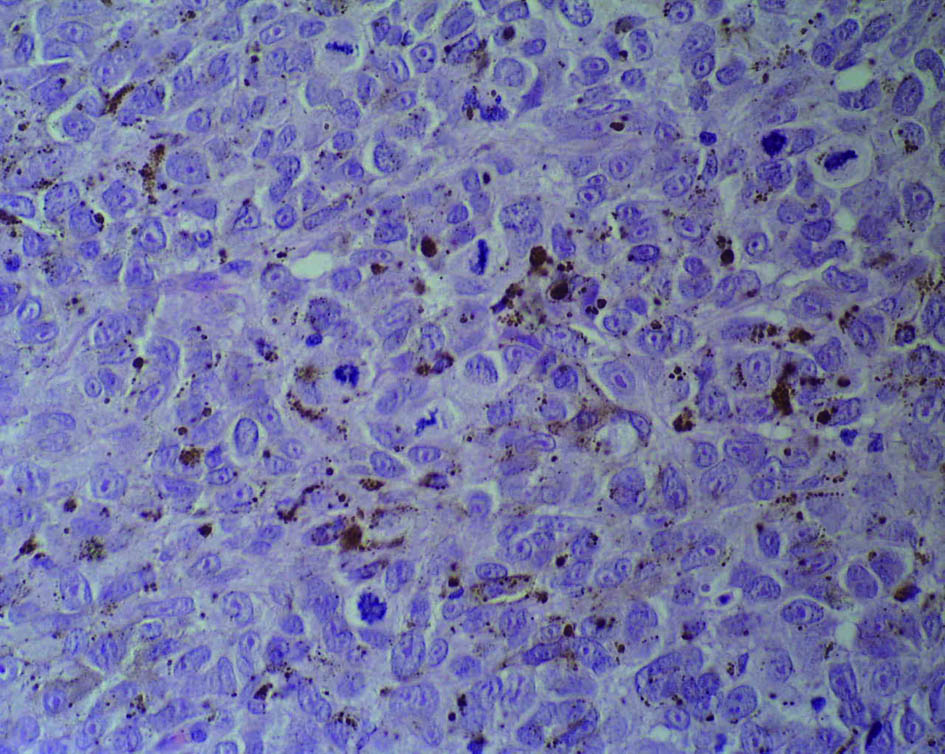 Click for large image | Figure 2. Nests of atypical melanocytes with the large nuclei showing prominent nucleoli, and numerous mitotic figures (hematoxylin and eosin stain ×400) |
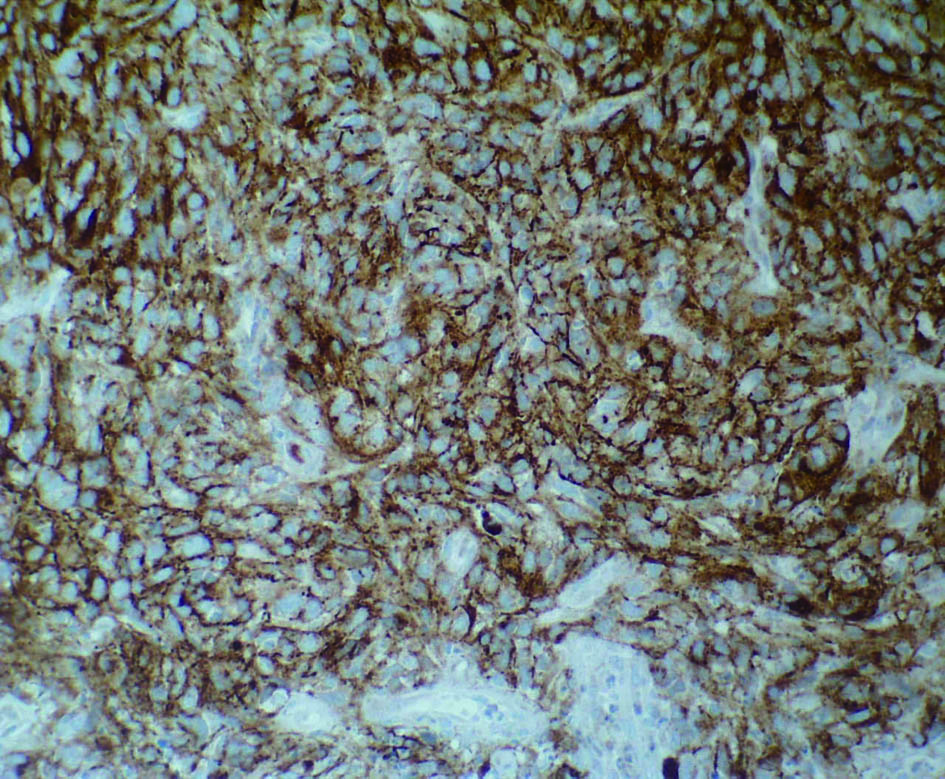 Click for large image | Figure 3. HMB-45 expression in melanoma cells (the immunohistochemical stain HMB-45, MSIP ×200) |
| Discussion | ▴Top |
Melanocytes are neural crest-derived cells located in the basal layer of skin, hair follicles, most squamous-covered mucosal membranes, leptomeninges and several other sites. Their function is to produce an insoluble pigment known as melanin using tyrosine as a substrate and to transfer this product through the process of cytocrinia to the adjacent epithelial cells. Ultrastructurally the hallmark of the melanocytes is the melanin-synthesizing organelle known as the melanosome [7]. Malignant melanoma is the tumour composed of atypical melanocytes. Histogenesis of melanomas arising in mucous membranes still remains in dispute and several theories have been proposed. In some animals it has been clearly demonstrated that melanoblast originating from the neural rests may subsequently migrate with mesodermal cells to sites where they usually not exist. A possible alternative mechanism is the so-called “melanogenic-metaplasia” of the epithelium, in other words metaplasia of squamous and glandular epithelium into pigment-producing cells. Finally neural crest elements may be transformed into melanocytes and nevus cells.
Primary malignant melanomas of the genitourinary tract are very rare tumours and represent less than 1% of all melanomas [8]. The tumour usually arises in the distal portion of the urethra. Symptoms of urethral melanomas rapidly develop and are not distinctive. They include urethral mass, nonspecific perineal pain, dysuria, frequency incontinence and hematuria or local bleeding [8]. The prognosis is poor. Metastases to the inguinal lymph nodes occur early in the course of the disease in 50% of the cases being already present at the time of the diagnosis. Rapid dissemination renders treatment very difficult in spite of an early diagnosis [8, 9].
The thickness of the tumour and the mitotic index have to be taken into account on microscopic examination, since tumours more than 1.5 mm thick and with more than one mitotic figure in every high power field carry a worse prognosis [9]. Metastatic melanoma should be excluded. The presence of junctional activity in the area adjacent to the lesion is of primary importance in this determination.
Two problems in planning the treatment should be recognized: local control and prevention of systemic disease. The local control is primarily surgical. This treatment included total uretherectomy with bilateral inguinal lymph node dissection as initial treatment in patients without evident distant metastases [9]. Some authors recommend even more radical therapy including pelvic exanteration in case of melanoma with depth of penetration more than 3 mm [9, 10]. Other authors suggest adjuvant treatment with β-interferon and systemic chemotherapy [10].
According to our knowledge 89 cases have been reported in literature, but only one reported survival longer than 6 years [10]. Despite adverse histological features revealed in our case (brisk mitotic activity, necrosis, depth of invasion) and conservative treatment, our patient is still alive and uneventful after 6 years. Therefore we presume that conventional histopathological prognostic factors do not play as important role in predicting outcome and biological behaviour in the primary malignant melanoma of the female urethra as in the primary skin melanomas.
Disclosure Statement
The authors declare that there are no conflicts of interest.
| References | ▴Top |
- Yoshizawa T, Kawata N, Sato K, Hirakata H, Igarashi T, Ichinose T, Yamaguchi K, et al. Primary malignant melanoma of the female urethra. Urology. 2007;70(6):1222 e1213-1226.
pubmed - Petersen Ro. Urologic pathology. JB Lippincott, Philadelphia, 1992.
- Poore RE, McCullough DL. Urethral Carcinoma. In: Gillenwater JY, Grayhalk JT, Howard SS (Eds). Adult And Pediatric Urology. Mosby, Missouri, 1996.
- Reed CAL. Melano-sarcoma of the female urethra: urethrectomy recovery. Am J Obstet Gynecol.1896; 34: 864-72.
- Nakamoto T, Inoue Y, Ueki T, Niimi N, Iwasaki Y. Primary amelanotic malignant melanoma of the female urethra. Int J Urol. 2007;14(2):153-155.
pubmed doi - Iversen K, Robins RE. Mucosal malignant melanomas. Am J Surg. 1980;139(5):660-664.
pubmed doi - Rosai J. Ackerman's surgical pathology. Mosby, St. Louis, 2004.
- Gupta R, Bhatti SS, Dinda AK, Singh MK. Primary melanoma of the urethra: a rare neoplasm of the urinary tract. Int Urol Nephrol. 2007;39(3):833-836.
pubmed doi - DiMarco DS, DiMarco CS, Zincke H, Webb MJ, Keeney GL, Bass S, Lightner DJ. Outcome of surgical treatment for primary malignant melanoma of the female urethra. J Urol. 2004;171(2 Pt 1):765-767.
pubmed doi - Oliva E, Quinn TR, Amin MB, Eble JN, Epstein JI, Srigley JR, Young RH. Primary malignant melanoma of the urethra: a clinicopathologic analysis of 15 cases. Am J Surg Pathol. 2000;24(6):785-796.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








