| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 1, February 2012, pages 4-6
Primary Abdominal Wall Actinomycosis
Seock Yeol Leea, c, Ji Hye Leeb, Seung Jin Leea, Cheol Sae Leea
aDepartment of Chest Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, South Korea
bDepartment of Pathology, Soonchunhyang University Cheonan Hospital, Cheonan, South Korea
cCorresponding author: Seock Yeol Lee, Soonchunhyang University Cheonan Hospital, 8, Soonchunhyang 2 gil, Dongnam-gu, Cheonan 330 - 721, South Korea
Manuscript accepted for publication September 19, 2011
Short title: Abdominal Wall Actinomycosis
doi: https://doi.org/10.4021/jmc336w
| Abstract | ▴Top |
Actinomycosis of the anterior abdominal wall is rare. We report a 50-year-old man who presented with a right lower lateral chest wall mass of six years duration Computed tomography showed a 8 cm mass projecting from right lower lateral chest wall associated with extension of the right abdominal wall. En bloc resection including muscles, 9th and 10th ribs and a partial portion of diphragm was made. And direct closure of abdominal wall defect was done. Histopathological examination of the mass was consistent with those of actinomycosis. The patient recovered completely without post-operative complications. The patient is receiving minocycline for three months now.
Keywords: Actinomycosis; Abdominal wall; Mass; Surgery
| Introduction | ▴Top |
Actinomycosis is a rare, chronic debilitating disease and it is difficult to diagnose and treat. Actinomycosis can involve almost any organ system but actinomycosis of the anterior abdominal wall is rare and follows recent abdominal organ surgery. We describe herein a rare primary anterior abdominal wall actinomycosis without abdomional organ involvement.
| Case Report | ▴Top |
A 50-year-old male complained of chest pain and an 8 cm sized mass in the right lower lateral chest wall that he had fist noticed 6 years previous to admission. There were no remarkable findings in his family and past history. His vital signs were stable and the results of routine blood tests were within normal ranges. Computer tomography (CT) indicated an 8 cm sized mass in the right lower hemithorax with extension of the right abdominal wall (Fig. 1). An isotope bone scan showed an increased hot uptake in the 9th rib (Fig. 2). We recommended preoperative culture and biopsy of the mass but the patient refused and wanted surgery for correct diagnosis and complete removal of mass. A 10 cm transverse skin incision was made on his mass area in the left lateral position under general anesthesia. There were inflammatory change on muscle, ribs and diaphragm. En bloc resection including latissimus dorsi muscle, external oblique muscle, intercostal muscles including 9th and 10th ribs and a partial portion of diaphragm was made. And direct closures of the diaphragm and abdominal wall defects were possible without prosthetic material. The cut surface of the resected specimen showed several necrotic areas in the fibrotic background on gross appearance. Microscopically, tangled clumps of filamentous organisms were found in the neutrophilic abscess. The filaments had a radial distribution. Neutrophils were adherent to the periphery of the colonies of organisms (Fig. 3). The microorganisms were consistent with diagnosis of actinomycosis. The patient was discharged on the seventh day after the operation following an uneventful recovery. The patient has been receiving minocycline for three months now due to positive penicillin skin test.
 Click for large image | Figure 1. Computer tomography showing about 8 cm mass projecting from right lower lateral chest wall associated with extension of the right abdominal wall (arrow). |
 Click for large image | Figure 2. Picture of bone scan showing hot uptake in right 9th rib (arrow). |
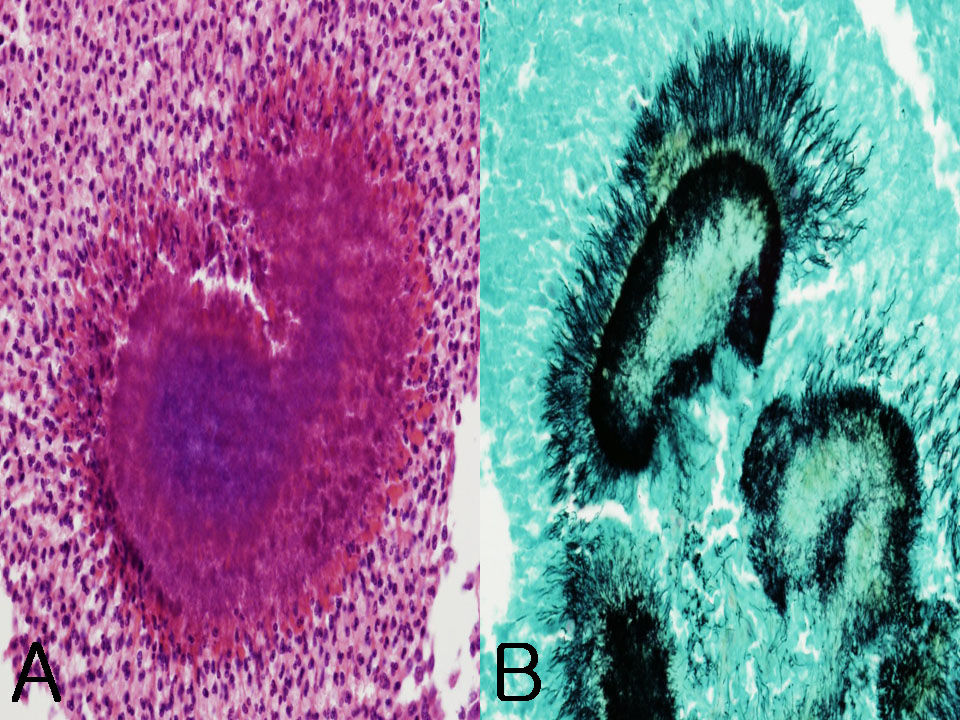 Click for large image | Figure 3. Microscopic appearance of the resected specimen. (A) Tangled clump of filamentous organisms in the abscess. Leukocytes adherent to the periphery of the clump (H&E, x 400). (B) Thin filamentous bacilli having a radial distribution or irregular clusters (Gomori methenamine silver stain, x 400). |
| Discussion | ▴Top |
Actinomycosis is a rare chronic, supporative pseudotumoral disease caused by an anaerobic gram positive organism that is most frequently Actinomyces Israeli [1]. In healthy subjects, Actinomyces is a part of normal flora of the oral cavity, the gastrointestinal tract and the genital tract. Healthy mucosa acts as a barrier to the spread of the organism, but tissues damaged by neoplasm, surgery, trauma, or foreign body allow multiplication and spread of actinomycosis [1]. Actinomycosis most commonly affects the head and neck (50%) but can involve almost any organ system [1]. Abdominopelvic actinomycosis is uncommon and typically follows recent bowel surgery such as procedures for acute appendicitis, diverticulitis or abdominal trauma [1].
Primary actinomycosis of the anterior abdominal wall is very rare and has been reported only in 29 cases in the literature by 2010 [2]. Immunocompromised status, such as diabetes mellitus, steroid therapy, and neoplasm, is a significant predisposing factor for actinomycosis [3].
Patients usually present with a slowly developing indolent swelling of the soft tissue. The disease usually presents as a slowly growing mass with eventual formation of sinuses discharging serosanguinous pus containing “sulfur” granules, which represent macrocolonies of actinomyocytes [3]. The “sulfur” granules are pathognomonic, but these are not always present [3]. In most cases, clinical and diagnostic exams are not able to identify the disease and therefore the treatment becomes complex. Hematological laboratory exams show elevated non specific inflammatory markers and serology is not diagnostic [4]. Ultrasonography, computed tomography or MRI do not suffice to differentiate between actinomycosis and other inflammatory or neoplastic processes [1].
It is also very difficult to isolate the bacterium from cultures [4]. Negative culture rate was reported to be 76% [3]. The most difficult task for the management of actinomycosis is to reach a diagnosis before a surgical approach. Preoperative diagnosis is difficult because of non-specific clinical, laboratory and imaging findings. In many cases, the diagnosis is often possible during surgical exploration or after extensive debulking [4].
This is the reason why a wide primary resection including the surrounding tissue is inevitable [1]. Operative management is required for diagnostic biopsy or total excision.
Surgery is necessary in many cases, especially when the mass is large or there are some complications such as peritonitis, compression of abdominal organ [4]. Surgery is also necessary when there is no benefit and general health conditions deteriorate after a week of antibiotic treatment [4].
The treatment of choice is proper surgical drainage at the primary site of infection. If a soft tissue tumor is suspected, a wide primary resection including the surrounding tissue is sometimes inevitable. The abdominal wall defect may be closed by prosthetic mesh if the abdominal wall defect is large and direct closure is impossible [1]. Surgical treatment without antibiotic therapy is not always sufficient to achieve a cure for actinomycosis. When antibiotic therapy is combined with surgery, it is relatively simple to treat and the cure rate is more than 90% [5]. Intravenous penicillin is the initial therapy of choice. In the case of penicillin allergy, tetracycline, erythromycin, clindamycin or minocycline are acceptable alternatives [6]. Our patient had positive penicillin skin test so, we started minocycline. The patient will take minocyline for six months.
Conflict of Interest
All authors declare that they have no conflict of interest.
| References | ▴Top |
- Ladurner R, Bogner JR, Drosse I, Volkmer E, Sommerey S, Hohenbleicher F, Wirth S, et al. A rare case of primary actinomycosis of the anterior abdominal wall: diagnosis and treatment. Hernia. 2008;12(5):549-552.
pubmed doi - Gomez-Ramirez J, Martin-Perez E, Alcaide B, Martin-Alvarez JL, Larranaga E. Primary abdominal wall actinomycosis. Cir Esp. 2009;85(4):256-258.
pubmed doi - Hefny AF, Joshi S, Saadeldin YA, Fadlalla H, Abu-Zidan FM. Primary anterior abdominal wall actinomycosis. Singapore Med J. 2006;47(5):419-421.
pubmed - Acquaro P, Tagliabue F, Confalonieri G, Faccioli P, Costa M. Abdominal wall actinomycosis simulating a malignant neoplasm: Case report and review of the literature. World J Gastrointest Surg. 2010;2(7):247-250.
pubmed - Das N, Lee J, Madden M, Elliot CS, Bateson P, Gilliland R. A rare case of abdominal actinomycosis presenting as an inflammatory pseudotumour. Int J Colorectal Dis. 2006;21(5):483-484.
pubmed doi - Kawahara M, Kawahara K, Goto T, Yamamoto S, Fuchinoue S, Matsumoto T. Abdominal actinomycosis misdiagnosed as a secondary bladder tumor: a case report. Int J Urol. 1998;5(5):498-500.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








