| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 12, December 2017, pages 383-387
Severe Takayasu Arteritis Complicated by Mesenteric Ischemia
Catarina Nunesa, d, Carlos Capelaa, Luisa Pintoa, Antonio Assuncaob, Ana Margarida Ferreirac
aDepartment of Internal Medicine, Hospital de Braga, Braga, Portugal
bDepartment of Vascular Surgery, Hospital de Braga, Braga, Portugal
cDepartment of Pathology, Hospital de Braga, Braga, Portugal
dCorresponding Author: Catarina Nunes, Rua Pedro Alvares Cabral 345, Santo Tirso, Portugal
Manuscript submitted October 20, 2017, accepted November 3, 2017
Short title: Takayasu Arteritis With Mesenteric Ischemia
doi: https://doi.org/10.14740/jmc2945w
| Abstract | ▴Top |
Takayasu arteritis (TA) is an idiopathic large vessel vasculitis which occurs mostly in young Asian females. The authors report an atypical presentation of TA in a woman who presented with signs and symptoms of limb claudication and mesenteric ischemia. This case illustrates the potential severity of this disease and the difficulty in its diagnosis and treatment. A 46-year-old Caucasian woman was admitted to the hospital with right lower limb claudication, aroused for small distances, in association to ischemic ipsilateral foot ulcers. She also reported recurrent episodes of abdominal pain, vomiting and diarrhea which leaded to an overall weight loss of 10 kg in a period of a year. Non-invasive vascular testing revealed a right ankle-brachial index of 0.17 and a left ankle-brachial index of 0.37. The abdominal aortography and the computed tomography (CT) angiography showed an occlusion of the superior mesenteric artery and irregularities of the aortic lumen. Oclusions in the right internal iliac artery and in the distal common femoral artery were found in the pelvic aortography. Lower limbs arteriography revealed multiple stenoses. The histological result from the femoral endarterectomy was consistent with large vessel vasculitis. The diagnosis of TA was established according to the American College of Rheumatology Criteria, based on the patient’s symptoms, physical and imaging findings. Despite aggressive immunosuppressive therapy with prednisolone and infliximab, an atypical refractory massive mesenteric ischemia occurred, leading to patient’s death. TA is a rare disease with variable presentation. Since this disease is associated with high morbidity and mortality, an early diagnosis is essential for the best prognosis. Critical mesenteric ischemia and peripheral limb ulcers are rare presentations. As mesenteric ischemia can be potentially fatal, early aggressive immunosuppressive therapy and resection of the affected bowel segment are usually required.
Keywords: Takayasu arteritis; Vasculitis; Rheumatology; Internal medicine; Vascular surgery
| Introduction | ▴Top |
Takayasu arteritis (TA) is a large-vessel chronic inflammatory vasculitis, mostly affecting large and medium sized arteries, with predilection for the aorta and its main branches. The inflammatory process results in stenosis, occlusion, dilation or aneurysm formation in the arterial wall [1, 2]. It is a rare disease with unknown etiology. Although the disease has a worldwide distribution, it appears to occur more often in young Asian women [3].
Patients with TA may present constitutional symptoms, vascular-ischemic pain with typical features such as lower limb claudication, decreased or absent peripheral pulses, vascular bruits, hypertension and reduction or discrepancies in blood pressure between arms [1, 2].
Epidemiological and mortality studies about TA are scarce but it is generally accepted that the survival of patients with TA is significantly lower than that observed in general population [4]. Medical treatment for TA includes glucocorticoids, immunosuppressants and new biological agents which are applied to patients with TA refractory to conventional treatment, with favourable results [5]. Efficacy of endovascular treatments for vascular complications, and consequently their indications, is still a matter of debate because of the high rate of restenosis at an early stage after the procedure [5].
The authors describe a case of TA which presented with signs and symptoms of limb claudication and mesenteric ischemia. This case reflects the severity of this disease and also the complexity in its diagnosis and treatment.
| Case Report | ▴Top |
A 46-year-old Portuguese Caucasian woman was admitted to the hospital with right lower limb claudication and non-infected ischemic ulcers on the second and third toes of right foot. Symptoms started 4 years before, with progressive worsening of right leg claudication, aroused for small distances 1 month before her admission.
Over the last year, she also described complaints of recurrent and transient episodes of severe abdominal pain, worsened after meals, accompanied with vomiting and diarrhea, with increasing intensity and frequency that led to an overall weight loss of 10 kg during that period. A Raynaud phenomenon on the third, fourth and fifth fingers of the left hand was also reported.
There was a relevant previous exposition to smoking habit (28 pack-unit years) and a consumption of about 40 g of alcohol per day. She denied hypertension, diabetes, dyslipidemia or surgical background. There were no regular medications.
On physical examination she was emaciated. The cardiopulmonary auscultation was normal. There were no bruits over both of the carotids, suprasternal and supraclavicular areas. Abdominal palpation was non-painful and no organomegaly or pulsating masses were found. No abdominal bruits were heard.
Right femoral pulse was less palpable than the left one. She had absent right popliteal and pedal pulses; weak left popliteal pulse and absent left pedal pulse. Left brachial, radial and ulnar pulses were very weak. Right upper extremity pulses were normal. The right ankle-brachial index (ABI) was 0.17 and left ABI was 0.37.
Laboratory investigations revealed a normocytic normochromic anaemia with an haemoglobin level of 10.4 g/dL (reference range 13.5 - 17.0 g/dL), white cell count 14.2 × 109/L (reference range 4.0 - 11.0 × 109/L) with 47% of neutrophils, platelet count 372 × 109/L (reference range 150 - 400 × 109/L), erythrocyte sedimentation rate (ESR) 13 mm/h (reference range 1.0 - 20.0 mm/h), and C-reactive protein (CRP) 2.9 mg/L (reference range < 2.9 mg/L). Renal, hepatic and thyroid functions were normal. Lipid profile was also normal. Serum protein electrophoresis did not reveal any change. Viral serology tests for human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV) and syphilis were negative. Bacterial and fungal blood cultures were negative. Autoimmune screening, including rheumatoid factor, anti-cyclic citrullinated peptide antibodies (anti-CCP), antinuclear antibodies (ANA), double-stranded DNA antibodies (dsDNA) and cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA) was also negative.
The transthoracic echocardiogram showed a patent foramen ovale that did not explain diffuse arterial changes. The abdominal aortography and CT angiography showed an occlusion in the distal third of the superior mesenteric artery and irregularities of the aortic lumen (Fig. 1). Pelvic aortography revealed occlusion of the right internal iliac artery and occlusion of the distal common femoral artery (Fig. 2). Lower limbs arteriography also showed multiple stenoses (Fig. 3). Doppler ultrasound of the left upper limb showed diffuse concentric thickening with multiple stenoses exceeding 50% of occlusion.
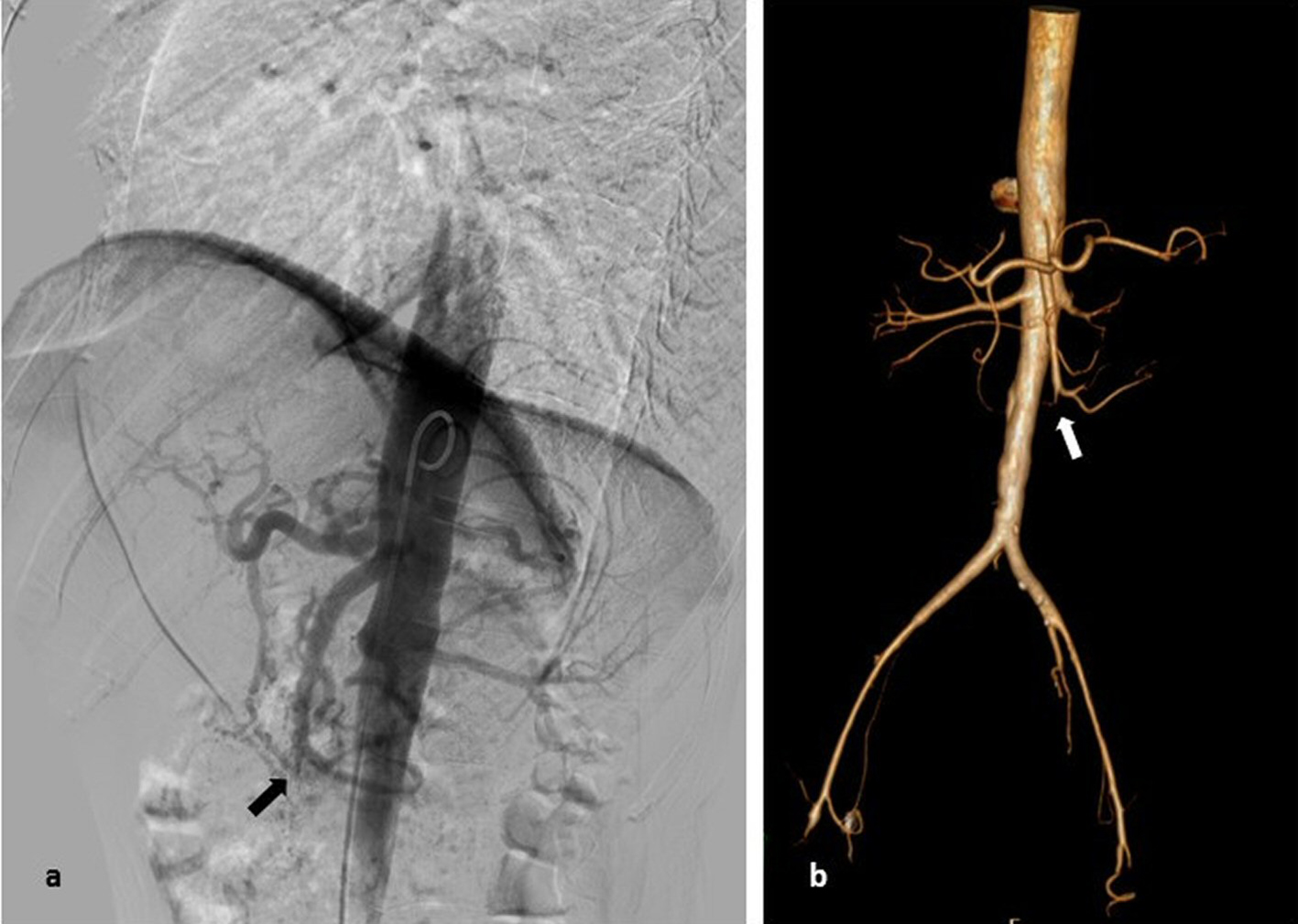 Click for large image | Figure 1. (a) Abdominal aortography: occlusion in the distal third of the superior mesenteric artery without collateral vascularization. (b) Abdominal CT angiography with 3D reconstruction: distal third occlusion of the superior mesenteric artery. |
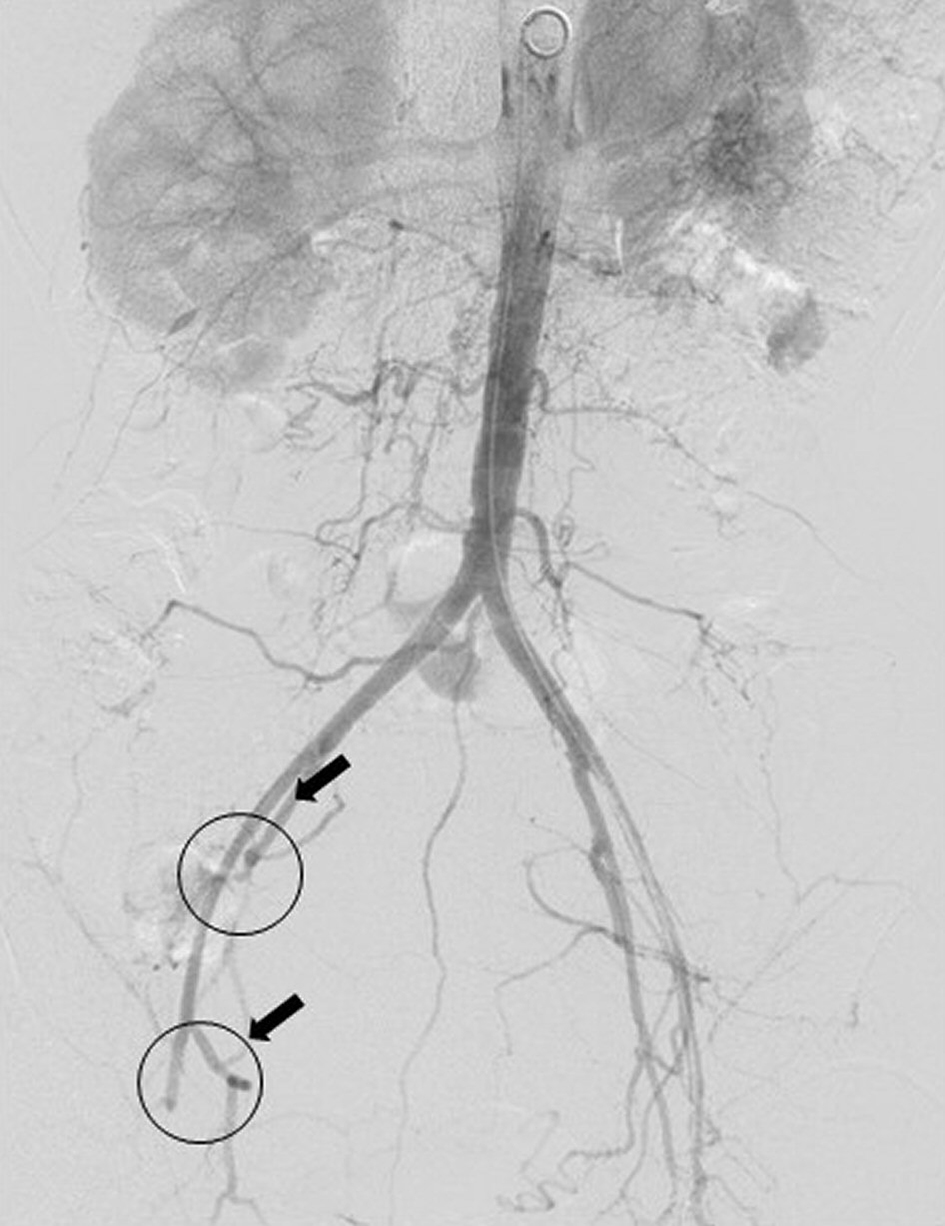 Click for large image | Figure 2. Pelvic aortography: irregularity of aortic lumen, occlusion of the right internal iliac artery and distal occlusion of the common femoral artery. |
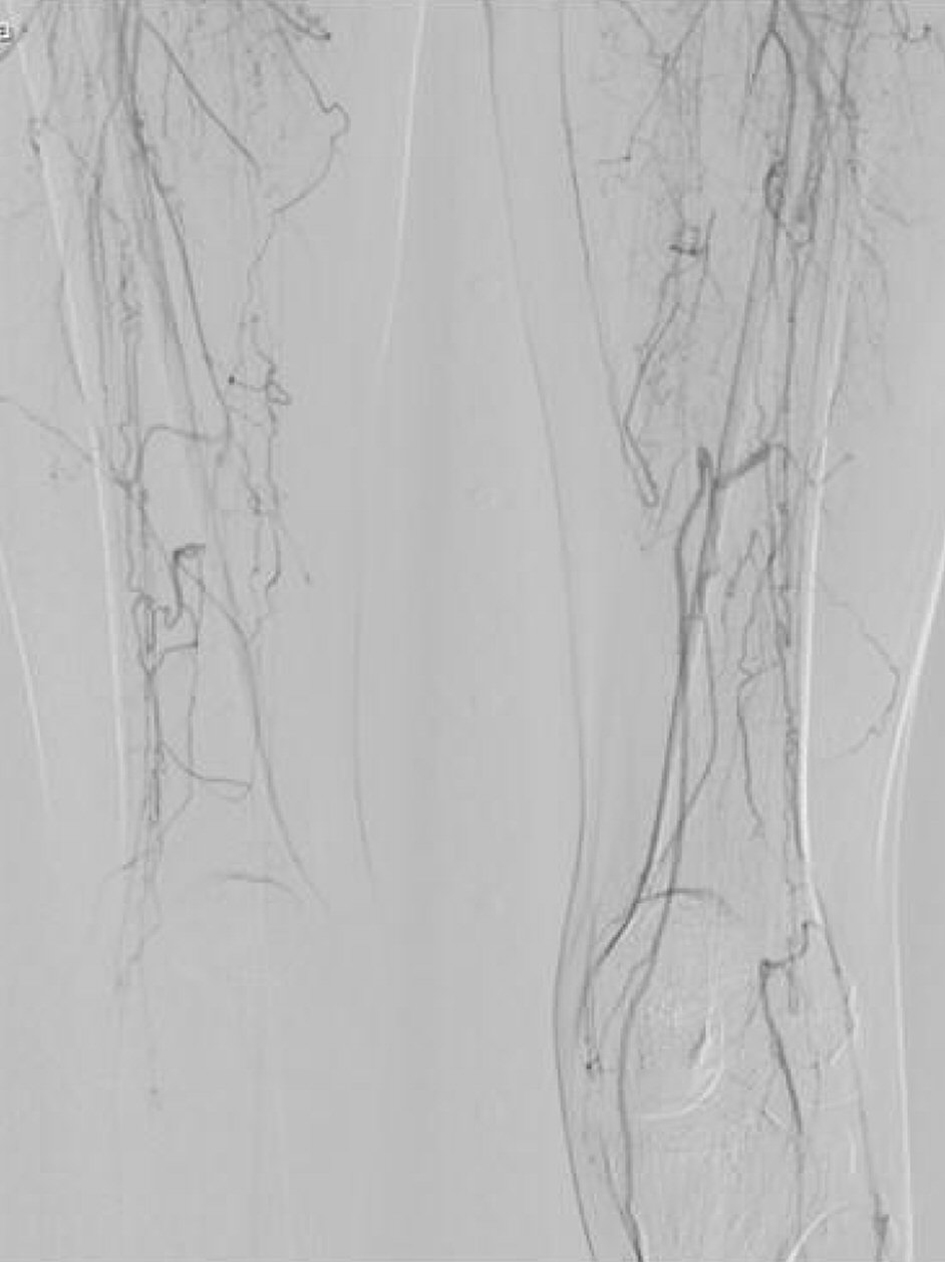 Click for large image | Figure 3. Arteriogrphy of the lower limbs: occlusion of the superficial femoral and popliteal arteries in the right and left limb. |
The diagnosis of TA was made according to the American College of Rheumatology 1990 criteria (claudication of extremities, decreased brachial artery pulse, blood pressure difference greater than 10 mm Hg and arteriogram abnormality).
Rescue immunosuppressive therapy with prednisolone was started (1 mg/kg/day), along with hypocoagulation with low-weight heparin, clopidogrel (75 mg/day) and pentoxifylline (400 mg thrice daily).
Despite medical treatment, persisting right foot pain as well as gradual worsening of ischemic ulcers led to an attempt of revascularization of the right femoral artery by surgical approach. Therefore, an open endarterectomy of the distal common femoral artery and a thromboembolectomy using a Fogarty balloon catheter were done. A thrombus and a small piece of the inner layer of the artery were collected. The histological result showed clots and an acute polymorphic inflammatory infiltrate suggesting a large vessel vasculitis (Fig. 4).
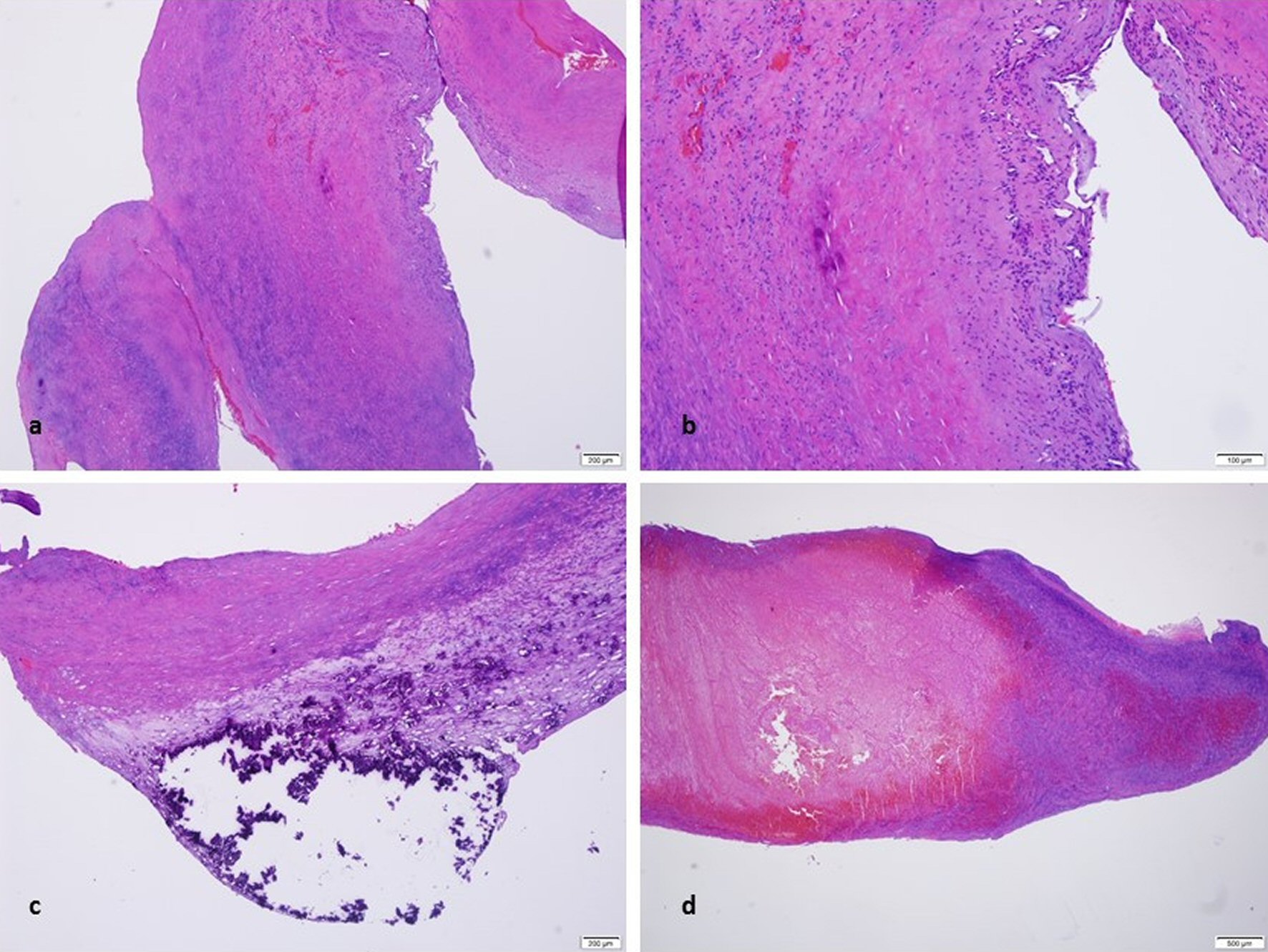 Click for large image | Figure 4. (a, b) Part of the wall of a blood vessel (H&E × 40) with acute inflammatory infiltrate (H&E × 100). (c) Calcifications of the wall of a blood vessel (H&E × 20). (d) Blood clot (H&E × 20). |
Although there was improvement in lower and upper limbs symptomatology, the persistence of abdominal pain and vomiting related to meals due to celiac-mesenteric vascular ischemia , lead to a more aggressive immunosuppressive strategy with an anti tumor necrosis factor (TNF) agent (infliximab 5 mg/kg).
In spite of aggressive medical treatment, refractory abdominal pain and vomiting worsened during hospitalization and the patient died 2 months after initial admission due to ischemic colitis consequent to inoperable mesenteric occlusion.
| Discussion | ▴Top |
TA is an idiopathic large and medium vessel vasculitis characterized by segmental chronic inflammation affecting predominantly aorta and its main branches [1, 2]. Annual estimated incidence is up to 3.3 cases per million in Asia compared to 0.4 - 1.3 cases per million in Europe [6]. The constant inflammatory process induces several degrees of stenoses, occlusions and dilatations of the involved vessels leading to ischemia and aneurysm formation [2].
TA presents with varied symptomatology, although it may be asymptomatic for a long time [3]. At an early stage, non-specific symptoms of inflammatory disease such as fever, night sweats, weight loss, malaise and arthralgia may appear and often anticipate more specific features. Usually narrowing vascular process is insidious allowing appropriate collateral vessel formation. As the disease advances, vascular occlusion may occur with symptoms related to the arterial affected area, which may include vertigo, syncope, stroke, limb claudication, angina, renovascular hypertension, abdominal pain and aortic dissection [1, 2, 7].
Critical mesenteric ischemia is an unusual manifestation of TA and may present with chronic and refractory abdominal pain [7, 8]. In a retrospective study with 126 patients diagnosed with TA only four had mesenteric ischemia as a manifestation of the disease [4]. Peripheral limb ischemia and gangrene are also extraordinarily uncommon with only 10 previous reported cases in literature [7, 9]. Concomitant intestinal and peripheral limb ischemia is extremely rare [7].
Elevation of inflammatory markers such as CRP or ESR is not pathognomonic for TA disease [2, 3]. According to data, at the time of diagnosis, inflammatory markers elevation can be found in only about 71% of the cases [4].
Establishing an early diagnosis is essential to the patient prognosis, since this disease is associated with high morbidity and mortality. Suspicion must be kept even when rare features are present, and a correct assessment of the vascular arterial area must be performed. Conventional angiography, which allows accurate assessment of vessel morphology and lumen, remains the gold standard for the diagnosis. CT angiogram and magnetic resonance angiography can also be used to evaluate large and medium size vessels [2, 3, 10].
In this case, clinical diagnosis of TA was based on American College of Rheumatology 1990 criteria, accomplishing four of the six criteria: claudication of extremities, decreased brachial artery pulse, difference of greater than 10 mm Hg in systolic blood pressure between arms and arteriogram abnormality. These classification criteria have a sensitivity and specificity of 90.5% and 97.7%, respectively [11]. Finally, the histological result was consistent with large vessel vasculitis.
Noteworthy in this case is the disease progression despite hypocoagulation, antiaggregation and immunosuppressive therapy with prednisolone. In about 50 % of the cases, isolated corticoid therapy is not sufficient to prevent vasculitis evolution and additional immunosuppressive therapy is required [2]. As in TA patient, the TNF-α level is increased, a vehement strategy with infliximab was instituted. The goal was to obtain the control of the disease in a fast and short time due to progressive degradation of the patient’s clinical status. Several studies have reported the efficiency of biological agents in the treatment of refractory TA patients [12-16]. This did not apply on this case. The past medical history of smoking habits may also have worsened the patient’s prognosis.
In conclusion, TA is a rare disease with variable presentation and nonspecific immunological laboratory profile. Establishing an early diagnosis is essential for a better prognosis, since this disease is associated with high morbidity and mortality. Critical mesenteric ischemia is an unusual manifestation of TA, nevertheless it can be a disastrous complication, requiring aggressive immunosuppressive therapy and usually involving resection of the affected segment of intestine. Multiple peripheral limb ulcers with consequent gangrene are extremely uncommon.
Conflict of Interest
We have no conflict of interest to declare.
Grant Support
None.
Author Contributions
CN is the first author and wrote the manuscript. AA and LP were involved in patient management and in writing the article. CC supervised the writing critically. AF performed the histological examination. All the authors have made significant contributions to this manuscript. All authors read and approved the final manuscript.
Consent
Written informed consent was obtained from the patient’s guardian for publication of this case report and for all the accompanying images.
| References | ▴Top |
- Johnston SL, Lock RJ, Gompels MM. Takayasu arteritis: a review. J Clin Pathol. 2002;55(7):481-486.
doi pubmed - Maffei S, Di Renzo M, Bova G, Auteri A, Pasqui AL. Takayasu’s arteritis: a review of the literature. Intern Emerg Med. 2006;1(2):105-112.
doi pubmed - Bryl M, Guzinski M, Rabczynski M, Waliszewska-Prosol M, Garcarek J, Adamiec R, Sasiadek M. Imaging difficulties in Takayasu arteritis - case report and review of the literature. Pol J Radiol. 2012;77(4):67-71.
doi pubmed - Schmidt J, Kermani TA, Bacani AK, Crowson CS, Cooper LT, Matteson EL, Warrington KJ. Diagnostic features, treatment, and outcomes of Takayasu arteritis in a US cohort of 126 patients. Mayo Clin Proc. 2013;88(8):822-830.
doi pubmed - Borg FA, Dasgupta B. Treatment and outcomes of large vessel arteritis. Best Pract Res Clin Rheumatol. 2009;23(3):325-337.
doi pubmed - Watts R, Al-Taiar A, Mooney J, Scott D, Macgregor A. The epidemiology of Takayasu arteritis in the UK. Rheumatology (Oxford). 2009;48(8):1008-1011.
doi pubmed - Misra DP, Krishnan N, Gochhait D, Emmanuel D, Negi VS. Takayasu arteritis (TA) first presenting with intestinal ischemia: a case report and review of gastrointestinal tract involvement (ischemic and non-ischemic) associated with TA. Rheumatol Int. 2017;37(1):169-175.
doi pubmed - Dewan R, Anuradha S, Sethi P, Ish P. Takayasu arteritis presenting as bowel gangrene: An unusual initial presentation. Arch Med Heal Sci. 2016;4(1):85.
doi - Misra DP, Chowdhury AC, Lal H, Mohindra N, Agarwal V. Gangrene in Takayasu’s arteritis: a report of two cases and review of literature. Rheumatol Int. 2016;36(3):449-453.
doi pubmed - Andrews J, Mason JC. Takayasu’s arteritis - recent advances in imaging offer promise. Rheumatology (Oxford). 2007;46(1):6-15.
doi pubmed - Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, Fauci AS, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33(8):1129-1134.
doi pubmed - Hoffman GS, Merkel PA, Brasington RD, Lenschow DJ, Liang P. Anti-tumor necrosis factor therapy in patients with difficult to treat Takayasu arteritis. Arthritis Rheum. 2004;50(7):2296-2304.
doi pubmed - Molloy ES, Langford CA, Clark TM, Gota CE, Hoffman GS. Anti-tumour necrosis factor therapy in patients with refractory Takayasu arteritis: long-term follow-up. Ann Rheum Dis. 2008;67(11):1567-1569.
doi pubmed - Schmidt J, Kermani TA, Bacani AK, Crowson CS, Matteson EL, Warrington KJ. Tumor necrosis factor inhibitors in patients with Takayasu arteritis: experience from a referral center with long-term followup. Arthritis Care Res (Hoboken). 2012;64(7):1079-1083.
doi - Comarmond C, Plaisier E, Dahan K, Mirault T, Emmerich J, Amoura Z, Cacoub P, et al. Anti TNF-alpha in refractory Takayasu’s arteritis: cases series and review of the literature. Autoimmun Rev. 2012;11(9):678-684.
doi pubmed - Quartuccio L, Schiavon F, Zuliani F, Carraro V, Catarsi E, Tavoni AG, Bombardieri S, et al. Long-term efficacy and improvement of health-related quality of life in patients with Takayasu’s arteritis treated with infliximab. Clin Exp Rheumatol. 2012;30(6):922-928.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








