| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 2, February 2017, pages 39-41
Radiotherapy for Inverted Papilloma of the Nasal Cavity: A Rare Case Report and Review of the Literature
Pinelopi Theopisti Memtsaa, e, Aikaterini Papadopouloub, Ariadni Kyriakogiannakic, Ioannis Tzitzikasb, Chrysoula Iliopouloud, Panagiotis Pantelisd, Martha Charalambidoud
aDepartment of Radiation Oncology, Cancer Hospital “Theageneio”, Thessaloniki, Greece
bDepartment of Radiation Oncology, AHEPA Hospital, Aristotle University, Thessaloniki, Greece
cDepartment of Radiation Oncology, Alexandra Hospital, Athens, Greece
dDepartment of Radiation Oncology, Cancer Hospital “Theageneio”, Thessaloniki, Greece
eCorresponding Author: Pinelopi Theopisti Memtsa, Department of Radiation Oncology, Cancer Hospital “Theageneio”, Thessaloniki, Greece
Manuscript accepted for publication December 23, 2016
Short title: RT for IP of Nasal Cavity
doi: https://doi.org/10.14740/jmc2735w
| Abstract | ▴Top |
Inverted papilloma or Schneiderian papilloma arising primarily from middle ear and mastoid is a very rare entity. It is a benign and locally aggressive condition, with increased risk of recurrence and malignant transformation. Surgery is the primary treatment and radiation therapy should be considered in case of malignant transformation, recurrent or inoperable disease. Here we report a case of recurrent inverted papilloma with dysplastic changes arising from nasal cavity in a 56-year-old male. The patient was treated with surgery followed by radiotherapy.
Keywords: Inverted papilloma; Radiation therapy; Sinonasal cavity
| Introduction | ▴Top |
Sinonasal inverted papilloma (IP) or Schneiderian papilloma is a neoplasm of epithelial lining origin which arises in the respiratory mucosa that lines the nasal cavity and paranasal sinuses. IP is best characterized by the male-to-female ratio of 3:1 with the peak incidence between fifth and sixth decade of life [1]. The inverted Schneiderian papilloma frequently appears as a unilateral lesion in the nasal septum and extends secondarily to the nasal and paranasal sinuses. IP represents uncommon benign neoplasm with an estimated incidence of 0.4-4.7% of all sinonasal tumors with locally aggressive behavior and increased risk of malignant transformation. Approximately, 11% of cases with IPs are associated with malignancies, most often of squamous cell histology [2]. The role of human papillomavirus (HPV) infection in the etiology of IP has been investigated of several studies. Thus, some of them consider HPV an important etiological factor, while others have not demonstrated any association [3]. The optimal therapeutic approach is surgical resection with main goal of the achievement of clear margins because of the high risk of repeat local recurrence. Radiotherapy of IP has proved to be effective in case of malignant transformation, recurrent or inoperable disease [1, 2]. Due to the rarity of the IP, there are very little evidence about long-term outcome and follow-up. In this study, we present a case of recurrent inverted papilloma in a 56-year-old man along with a review and discussion of the literature to date.
| Case Report | ▴Top |
A 56-year-old man was referred to our hospital with a history of IP of the right nasal cavity, since 1982. For that reason, he underwent a surgical excision twice due to recurrences. According to the histological report, it was an IP with negative surgical margins. He reported a few months history of right-sided facial pain and pressure, nasal fullness and epistaxis. In the context of his follow-up, the patient underwent a CT, where there was a soft tissue mass in the superior wall of the right maxillary sinus with invasion to the right walls and the floor of the right orbit (Figs. 1 and 2). The disease extent and the invasion of adjacent structures were determined with the help of MRI. Contrast-enhanced magnetic resonance imaging (MRI) revealed a 6.5 × 6 × 3 cm tumor mass involving the sphenoid sinuses, nasal cavity, ethmoidal cells and the floor of the right orbit. Under general anesthesia, the patient underwent an extensive resection with orbital preservation via a right lateral rhinotomy approach. Surgery with negative margins was not possible. The sample was sent to the oral pathology laboratory and analyzed by routine procedure, with slides stained using the hematoxylin-eosin technique. The histopathological analysis revealed papilliferous projections lined by keratinized and non-keratinized squamous epithelium, with invagination areas directed to the stroma and koilocytes in the superficial layers. In some of the basal and parabasal layer areas, hyperchromatic cells could be observed, with voluminous nuclei and scarce cytoplasm and mitotic figures. The connective tissue was edematous. Vascular congestion and discreet mononuclear inflammatory infiltrate were also observed. He was referred to the Radiotherapy Department for adjuvant radiation therapy (RT) with a total dose volume of 54 Gy in 30 sessions with a daily dose volume of 1.8 Gy. The radiotherapy was performed in a linear accelerator with 6 MV energy and 0.5 cm margin from the bed of the tumor. Acute radiation mucositis and dermatitis were observed, both of which were classified as grade 2. The patient was followed up 1 month later with clinical examination and his mucositis and dermatitis resolved.
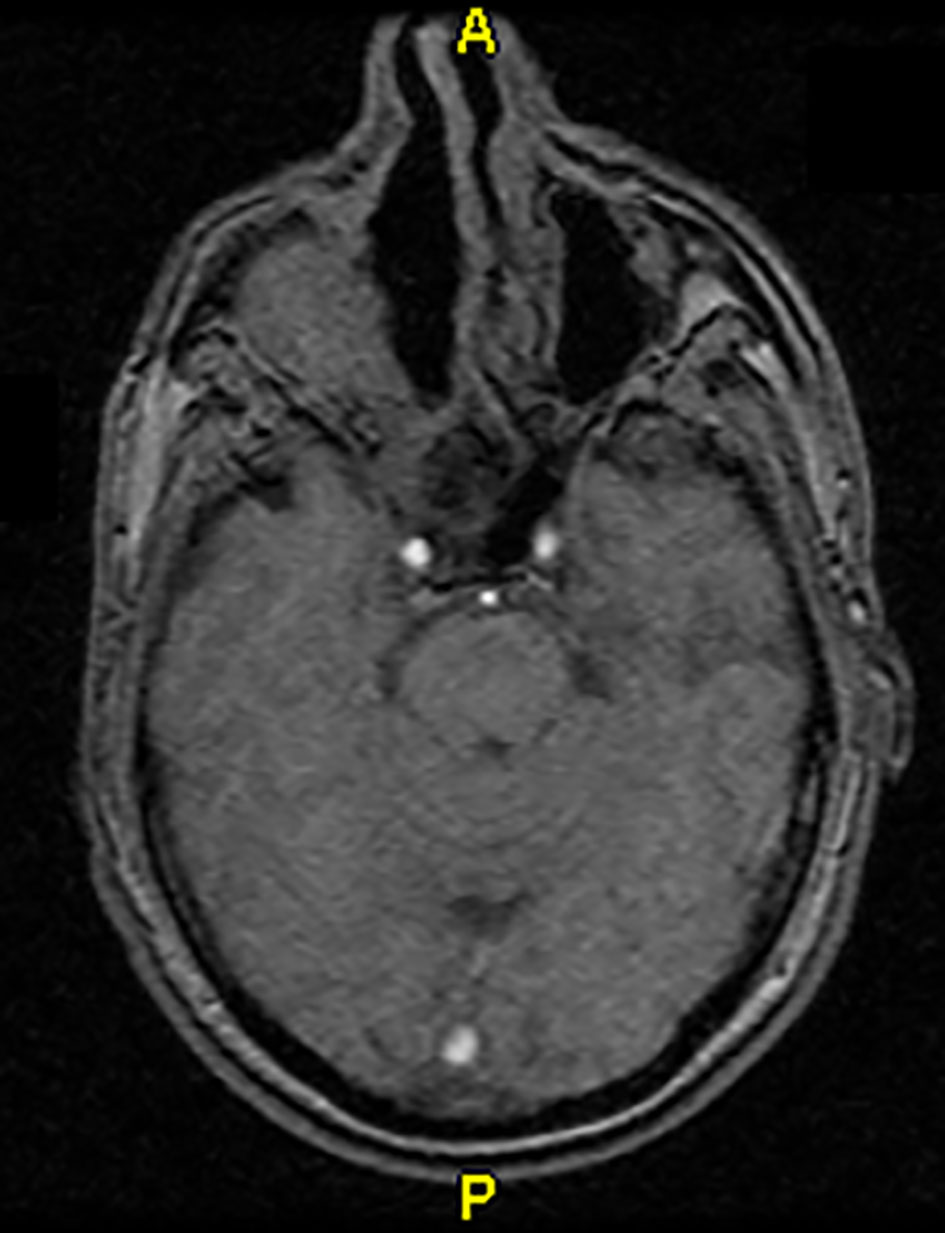 Click for large image | Figure 1. MRI after surgery. |
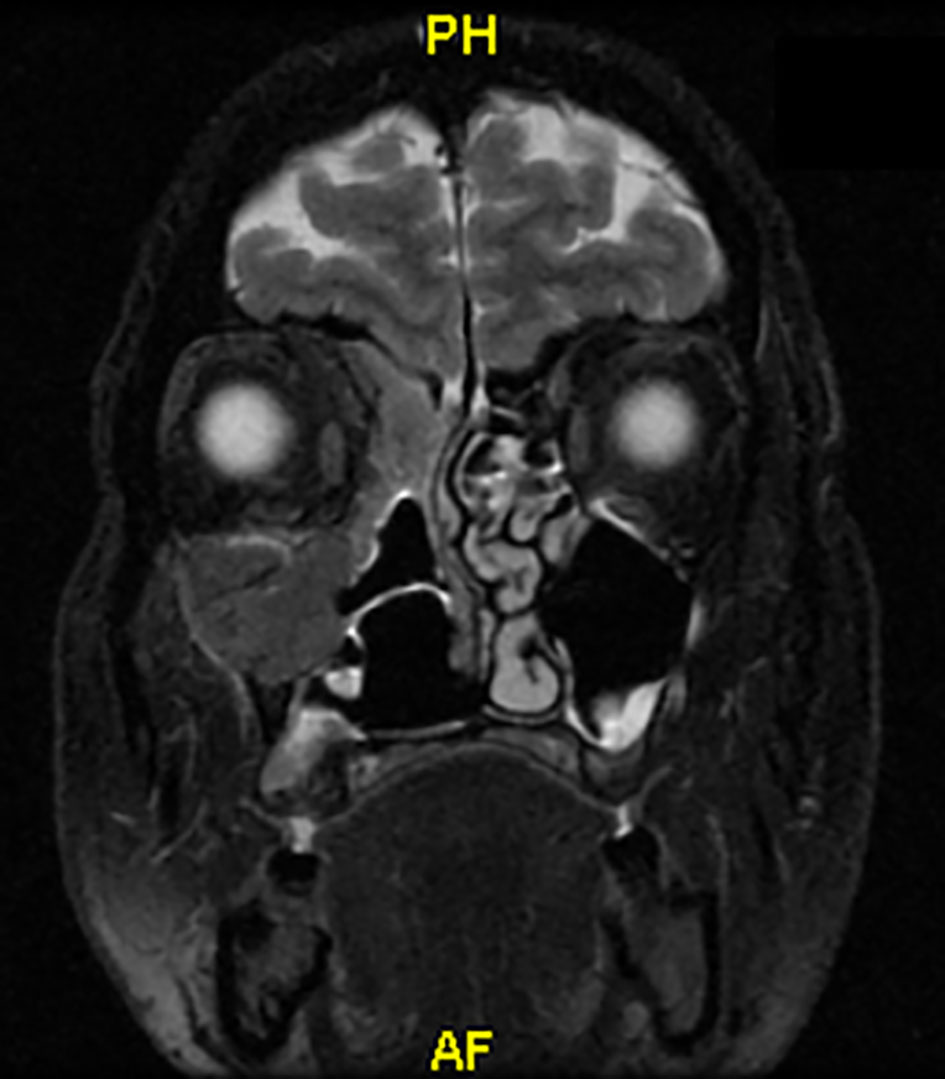 Click for large image | Figure 2. Coronary MRI before radiotherapy. |
| Discussion | ▴Top |
Sinonasal IP is extremely rare, accounting for approximately 0.4-4.7% of all sinonasal tumors; therefore, it is very rarely encountered in the everyday clinical practice. IP arises from lining epithelium of nasal cavity and paranasal sinus which is also known as Schneiderian epithelium. Histologically three types of papillomas have been identified: exophytic papilloma, oncocytic papilloma and IP, out of which IP is the commonest (62%) and can be lined by squamous, transitional or respiratory epithelium [4]. MRI is preferred in diagnosis and follow-up because of its sensitivity and specificity for differentiating soft tissue mass from postoperative changes and inflammation. Although IP is benign, it reduces the patient’s quality of life due to compromised nasal function, extension to the orbit and paranasal sinus. Three typical characteristics of IP include a high propensity of recurrence, local aggressiveness and association with malignancy. Hence, surgical resection is the mainstay of treatment [5]. However, large masses or those involving adjacent critical structures often cannot be completely resected due to esthetic considerations or functional reasons. Strict attention must be paid to identifying the site of tumor attachment and aggressive resection of a margin of mucosa and bone at this location. Although many initial IP lesions are unifocal, inadequate tumor removal promotes multifocality. A unilateral mass with a lobulated pattern is a common radiographic feature of tumor recurrence [6]. Recurrence occurring despite radical resection may result from the multicentric nature of the papilloma. Most recurrences occur at the margins of previous surgical resections within the first few years of therapy, but 17% of the patients have late recurrences after 5 years. Postoperative RT should be considered in case of malignant histology and incomplete resection [7]. RT can also be considered in cases of recurrent and inoperable disease. In the past, radiotherapy has only been used on exception in the treatment of histologically overt benign IPs. Due to the risk of anaplastic transformation after treatment with irradiation, many authors in the past advocated avoiding the use of RT in this benign disease. The second reason, also originated in the past when imaging and RT were much less sophisticated and effective than nowadays, would be the opinion that RT is ineffective in preventing recurrences. Recently, modern radiologic techniques allow even better visualization of the extent of tumors and more effective planning of surgical procedures [8]. In review of the literature for irradiation of benign IPs, we found only six studies with, in total, 16 patients describing necessary details on therapy and outcome. Indications for irradiation were inoperability, due to the extent of the tumor or medical comorbidities, incomplete resection or history of multiple recurrences of otherwise benign tumor. When only those patients, after gross or subtotal tumor resection from are considered, RT failed in two out of 14 cases. The two were irradiated to 57.4 and 50 Gy [9]. In patients who were locally controlled, the lowest and the median dose were 47.15 and 56.5 Gy, respectively, and the follow-up period ranged between 0.5 and 20.5 years. It seems that in benign IPs, RT with doses ranging from 50 Gy to well below 60 Gy effectively prevents tumor re-appearance when there is no residual or only a small residual left behind after surgery. If tumor burden is extensive, e.g. when no surgical debulking is carried out, irradiation doses in the range of 70 Gy appear to be indicated [10].
Importantly, the RT dose that was used in our case (54 Gy in 30 fractions of 1.8 Gy per day) is still in the range of doses closer to a “near zero” incidence of RT-induced optic neuropathy, which makes RT acceptable also from a morbidity point of view. Because only two cases with neck metastases of benign-appearing IPs have been reported so far, no elective irradiation of regional lymphatics is needed. In order to improve the therapeutic outcomes, novel RT techniques have been proposed, including intensity-modulated RT with image guidance, and hyperfractionation of RT dose with increased dose conformity [7, 8].
To conclude, in histologically benign IPs, RT is safe and is indicated when the risk of tumor recurrence after surgery is increased, either due to subtotal resection or a history of recurrent disease, and in inoperable tumors. Moderate RT doses well below 60 Gy can effectively prevent recurrence after gross or subtotal resection whereas for inoperable tumors doses in the range of 70 Gy are indicated.
Conclusion
Sinonasal adverted papilloma is a rare benign disease. Early aggressive surgical management with adjuvant RT may help to recurrences. Because of the higher tendency of recurrence and malignant transformation, the patients of IP should be considered for long-term follow-up. Besides clinical examination, MRI should be performed during the follow-up. More multicenter randomized trials with long-term follow-up should be performed so as to have evidence about the sequence of the treatments and the role of RT in this benign disease.
| References | ▴Top |
- Pitak-Arnnop P, Bertolini J, Dhanuthai K, Hendricks J, Hemprich A, Pausch NC. Intracranial extension of Schneiderian inverted papilloma: a case report and literature review. Ger Med Sci. 2012;10:Doc12.
pubmed - Eggers G, Muhling J, Hassfeld S. Inverted papilloma of paranasal sinuses. J Craniomaxillofac Surg. 2007;35(1):21-29.
doi pubmed - Jenko K, Kocjan B, Zidar N, Poljak M, Strojan P, Zargi M, et al. In inverted papillomas HPV more likely represents incidental colonization than an etiological factor. Virchows Arch. 2011;459:29-38.
doi pubmed - Oikawa K, Furuta Y, Itoh T, Oridate N, Fukuda S. Clinical and pathological analysis of recurrent inverted papilloma. Ann Otol Rhinol Laryngol. 2007;116(4):297-303.
doi pubmed - Anari S, Carrie S. Sinonasal inverted papilloma: narrative review. J Laryngol Otol. 2010;124(7):705-715.
doi pubmed - Coca-Pelaz A, Gomez-Martinez J, Vivanco-Allende B, Hermsen M, Llorente JL. Primary inverted papilloma of the middle ear with intracranial invasion. Head Neck. 2016;38(5):E105-107.
doi pubmed - Hug EB, Wang CC, Montgomery WW, Goodman ML. Management of inverted papilloma of the nasal cavity and paranasal sinuses: importance of radiation therapy. Int J Radiat Oncol Biol Phys. 1993;26(1):67-72.
doi - Gomez JA, Mendenhall WM, Tannehill SP, Stringer SP, Cassisi NJ. Radiation therapy in inverted papillomas of the nasal cavity and paranasal sinuses. Am J Otolaryngol. 2000;21(3):174-178.
doi - Vorasubin N, Vira D, Suh JD, Bhuta S, Wang MB. Schneiderian papillomas: comparative review of exophytic, oncocytic, and inverted types. Am J Rhinol Allergy. 2013;27(4):287-292.
doi pubmed - Vrabec DP. The inverted Schneiderian papilloma: a 25-year study. Laryngoscope. 1994;104(5 Pt 1):582-605.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








