| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 8, August 2016, pages 344-347
Acidotic Hypercapnia: A Case Series of Acidosis Driven Respiratory Muscle Dysfunction
Catherine Kinga, Abigail Bishoppa, Natasha Santana-Vaza, Ambika Talwara, Rahul Mukherjeea, b
aDepartment of Respiratory Medicine, Heart of England NHS Foundation Trust, Birmingham, UK
bCorresponding Author: Rahul Mukherjee, Department of Respiratory Medicine & Physiology, Birmingham Heartlands Hospital, Bordesley Green East, Birmingham, B9 5SS, UK
Manuscript accepted for publication June 17, 2016
Short title: Acidotic Hypercapnia
doi: http://dx.doi.org/10.14740/jmc2542e
| Abstract | ▴Top |
Established indications for non-invasive ventilation (NIV) include acute or acute-on-chronic type 2 respiratory failure associated with acidosis. It is commonly assumed that this acidosis is a secondary phenomenon which follows the development of acute hypercapnia. This case series describes four patients with acidotic hypercapnia (type 2 respiratory failure secondary to metabolic acidosis) demonstrated through serial arterial blood gases who were successfully treated with NIV. Acidotic hypercapnia is a relatively common under-recognized subtype of respiratory failure for which further trials are required to establish the role of NIV.
Keywords: Metabolic acidosis; Non-invasive ventilation; Type 2 respiratory failure
| Introduction | ▴Top |
There is now a substantial evidence base demonstrating the efficacy of non-invasive ventilation (NIV) in patients who develop hypercapnic respiratory failure associated with acidosis, predominantly in those with chronic obstructive pulmonary disease (COPD) [1, 2]. However, there is a paucity of information about 1) whether the hypercapnia caused a respiratory acidosis (hypercapnic acidosis) as classically occurs with COPD; 2) whether metabolic acidosis led to hypercapnia (acidotic hypercapnia); and 3) whether the management of patients with acidotic hypercapnia should differ from those with hypercapnic acidosis. This distinction between hypercapnic acidosis and acidotic hypercapnia is possible through a time series of arterial blood gas (ABG) measurements. This case series describes four patients with acidotic hypercapnia who were treated successfully using ward-based NIV within our 11-bedded NIV unit.
| Case Reports | ▴Top |
Case 1
A 64-year-old housewife with type 2 diabetes mellitus (on metformin) and a background ventilatory insufficiency due to COPD (FEV1 1.19 L (61% predicted)) was admitted with right upper lobe pneumonia and a non-ST-elevation myocardial infarction (NSTEMI). Initial ABG demonstrated a metabolic acidosis (FiO2 28%: pH 7.336, PaCO2 5.56, PaO2 11.2, HCO3 20.8, lactate 1.4) (Fig. 1). Despite standardized treatment for her pneumonia and NSTEMI, a repeat ABG revealed worsening metabolic acidosis with onset of hypercapnia (FiO2 24%: pH 7.293, PaCO2 6.39, PaO2 16.2, HCO3 20.8, lactate 1.5). The following day, NIV was commenced due to further deterioration (FiO2 24%: pH 7.143, PaCO2 11.8, PaO2 8.76, HCO3 22.8, lactate 2.7) and dyspnea. The patient was successfully weaned the following day (FiO2 21%: pH 7.462, PaCO2 5.7, PaO2 7.91, HCO3 29.8, lactate 0.9). This patient did not required further hospital admission in the following 2 years.
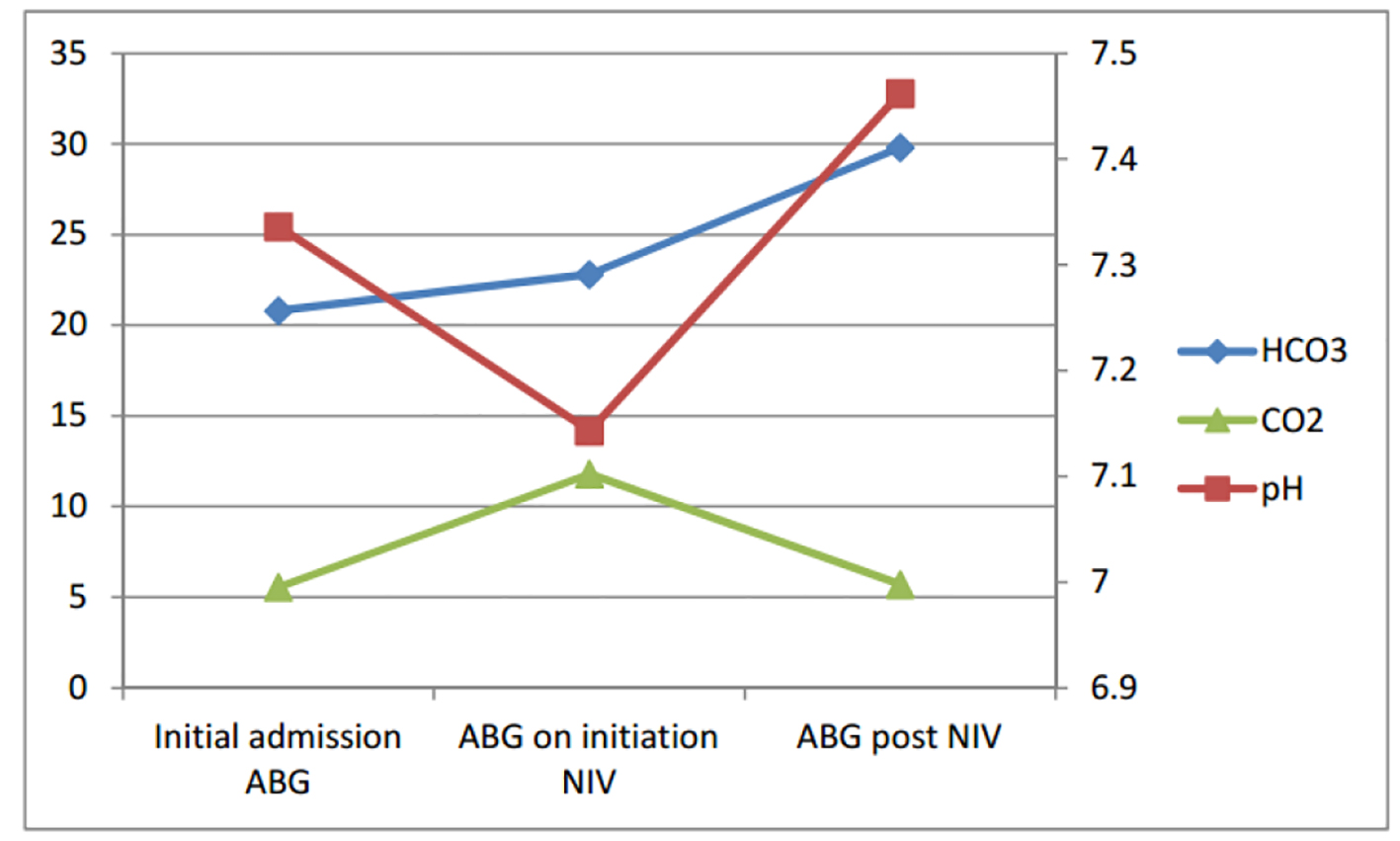 Click for large image | Figure 1. Serial ABGs for case 1. |
Case 2
A 75-year-old retired male motor industry worker with moderate COPD (FEV1 1.29 L (57% predicted)) was admitted with breathlessness secondary to congestive cardiac failure (known left ventricular ejection fraction 15%). Applying the Henderson-Hasselbalch equation to his ABG (pH 7.06, PaCO2 12.0, PaO2 8.55, HCO3 17.9), for his PaCO2 value, a bicarbonate of 24.6 mmol/L was expected, not 17.9 mmol/L, confirming a picture of metabolic acidosis [3] (Fig. 2). After receiving NIV, his acidotic hypercapnia completely resolved within 24 h (pH 7.43, PaCO2 5.10, PaO2 8.11, HCO3 25.4). The speed of recovery was suggestive of transient respiratory muscle/drive impairment in comparison to that seen with hypercapnic acidosis in COPD. Again, he had no further respiratory admissions in the succeeding year.
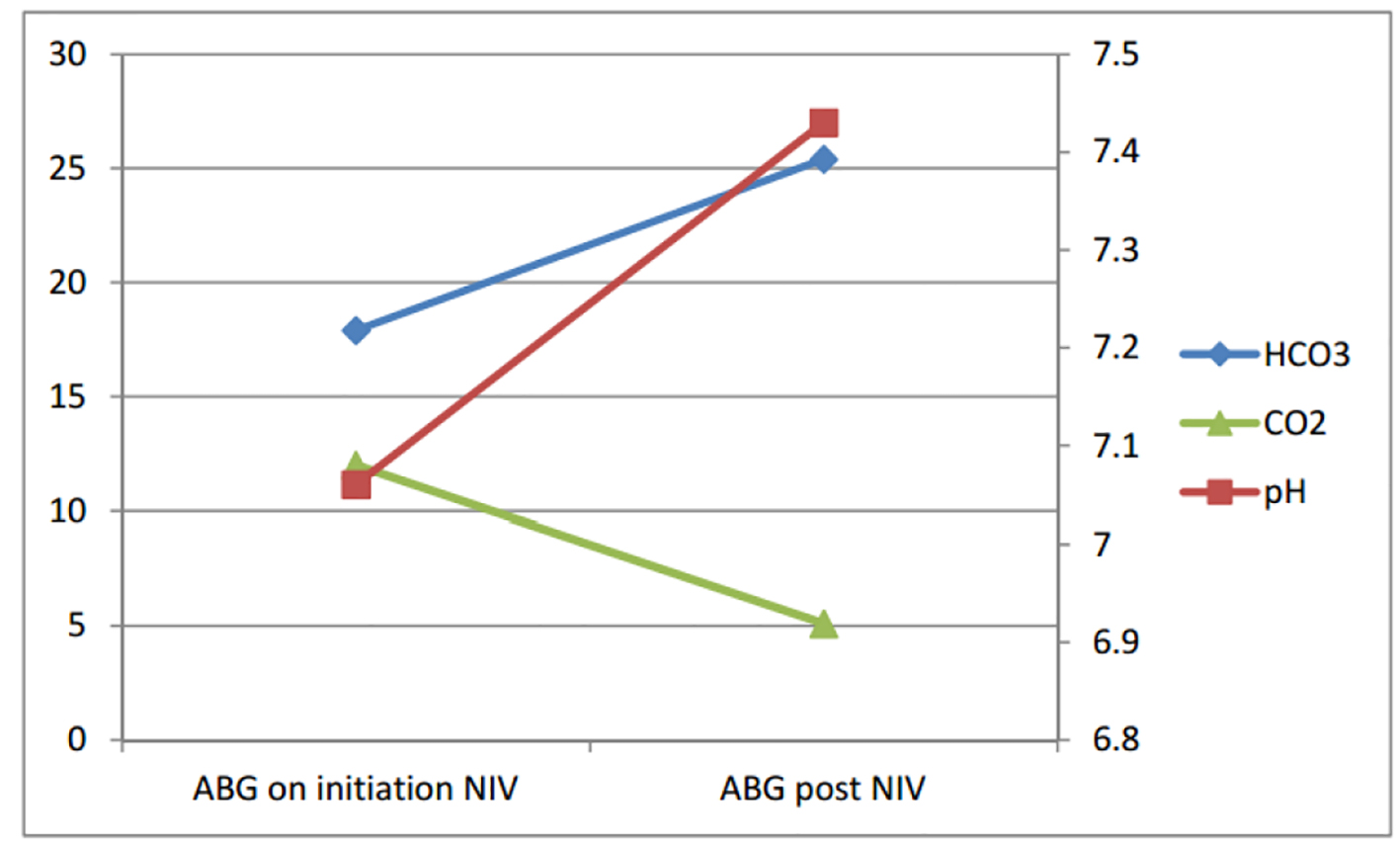 Click for large image | Figure 2. Serial ABGs for case 2. |
Case 3
A 78-year-old retired female car factory worker with severe COPD (FEV1 = 0.75 L (43% predicted)) was admitted with shortness of breath, productive cough and pyrexia. Initial ABG revealed a metabolic acidosis (FiO2 0.5 L: pH 7.30, PaCO2 6.06, PaO2 8.73, HCO3 20.8) and she was treated for an acute exacerbation of COPD (AECOPD) with antibiotics, steroids and oxygen (Fig. 3). Despite an initial response to therapy, serial ABGs demonstrated progressing hypercapnia (FiO2 4 L: pH 7.066, PaCO2 12.3, PaO2 8.52, HCO3 18.2) for which the patient was commenced on NIV and transferred to HDU in view of respiratory fatigue. The patient, however, responded well to NIV with complete reversal of her acidotic hypercapnia (FiO2: 21%: pH 7.458, PaCO2 6.12, PaO2 7.48, HCO3 31.1).
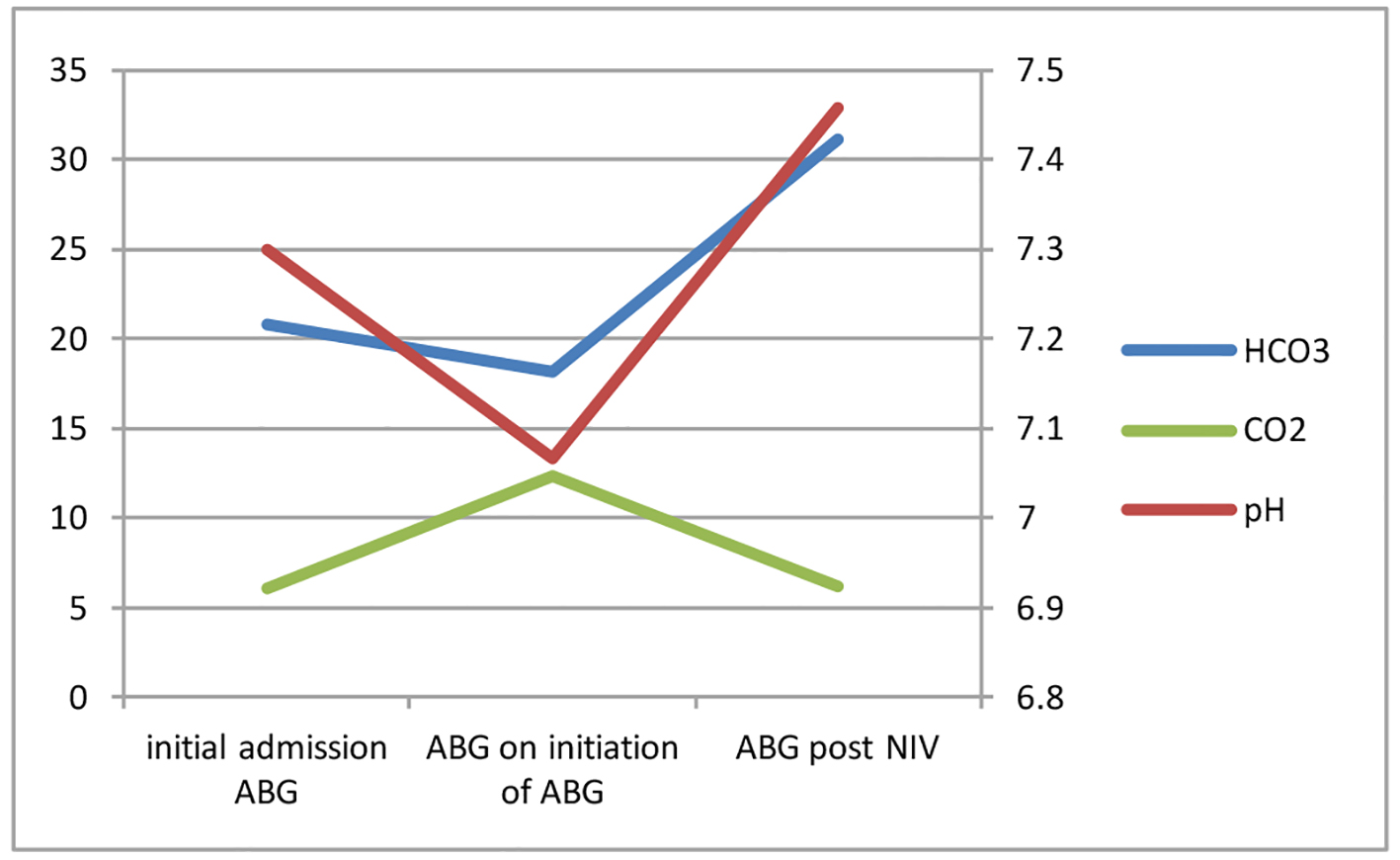 Click for large image | Figure 3. Serial ABGs for case 3. |
Case 4
A 60-year-old housewife with background ventilatory insufficiency secondary to a BMI 41.9 kg/m2 and a history of chronic kidney disease was admitted with drowsiness, confusion and agitation. Having recently been diagnosed with mumps, she was initially covered with intravenous acyclovir as well as clarithromycin and benzylpenicillin. ABG on admission demonstrated a mixed respiratory and metabolic acidosis due to a combination of undiagnosed obstructive sleep apnea (OSA) and non-steroidal anti-inflammatory drug (NSAID) induced acute-on-chronic renal failure (pH 7.224, PaCO2 5.93, PaO2 11.5, HCO3 17.2) (Fig. 4). Serial ABG measurements demonstrated a worsening hypercapnia for which NIV was commenced (pH 7.26, PaCO2 8.0, PaO2 10.3, HCO3 23.6) achieving a rapid reversal (pH 7.464, PaCO2 4.75, PaO2 9.43, HCO3 21.8). In-patient sleep studies confirmed severe OSA with an apnea/hypopnea index 120.8/h; nocturnal CPAP was commenced prior to discharge.
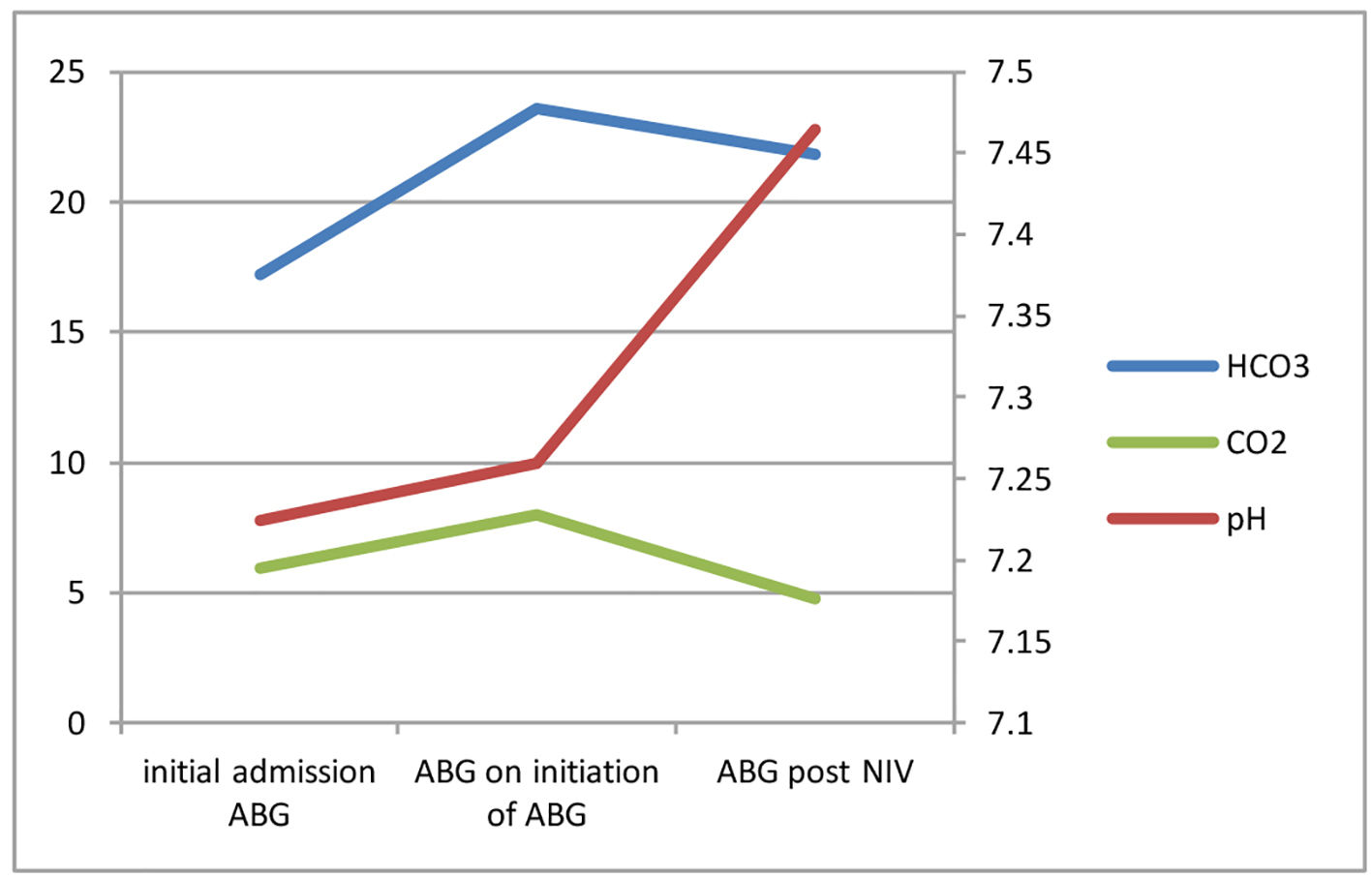 Click for large image | Figure 4. Serial ABGs for case 4. |
| Discussion | ▴Top |
This case series describes four patients with varying degrees of ventilatory insufficiency who received NIV to treat acidotic hypercapnia. ABG time series in cases 1, 3 and 4 demonstrate a rising PaCO2 following the onset of a metabolic acidosis whilst case 2 exhibits inappropriately low bicarbonate for a diagnosis of respiratory acidosis, again suggesting that metabolic acidosis preceded the onset of hypercapnia. In all four cases, the acidotic hypercapnia was reversed completely following initiation of NIV alongside optimal medical management with fluid resuscitation and the treatment of sepsis. These patients all remained well following discharge which arguably differs from the natural course of patients with COPD requiring NIV, who typically necessitate repeated hospital admissions.
At present, respiratory failure is widely categorized as either type 1 (hypoxemia) or type 2 (hypoxemia with an associated hypercapnia). Previous prospective randomized trials demonstrating the efficacy of NIV in patients with type 2 respiratory failure secondary to an AECOPD, used the pH as the primary indicator of the acuity of the respiratory failure (without reference to the serum bicarbonate concentration) [1]. Therefore, patients with type 2 respiratory failure secondary to metabolic acidosis, as described in this case series, were not previously recognized as a subgroup.
Metabolic acidosis is common in those with hepatic, renal or cardiac dysfunction and is frequently observed in patients admitted with acute medical problems (including AECOPD). Patients with underlying respiratory disease may develop hypercapnia with a metabolic acidosis due to inadequate respiratory compensation following stimulation of peripheral chemoreceptors [3]. Acidosis is a recognized cause of muscular dysfunction and may contribute to respiratory muscle fatigue especially in patients with underlying respiratory pathology [4]. Additionally, there is recognition of a similar causation of respiratory failure in the critical care literature due to circulatory shock causing type 4 respiratory failure which resolves when shock is corrected [5].
A recent UK audit demonstrated that patients with AECOPD are receiving NIV in the presence of mixed metabolic and respiratory acidosis (although acidotic hypercapnia was not described), and those with bicarbonate below 23 mmol/L have a higher mortality than those with normal/high bicarbonate [6]. However, at present, there are insufficient data to suggest whether and how long NIV should be used in these circumstances.
Although further trials are required to decide what the best treatment for this important subset of patients with acidotic hypercapnia is, we would wish to emphasize the importance of monitoring for hypercapnia in patients admitted with a metabolic acidosis, particularly in the presence of background ventilatory insufficiency. Equally, we would wish to underline the importance of the fluid/sepsis management in those admitted acutely for NIV with hypercapnia and acidosis. Further research about the etiopathogenesis of acidotic hypercapnia would further guide the medical management of this patient cohort.
| References | ▴Top |
- Roberts CM, Brown JL, Reinhardt AK, Kaul S, Scales K, Mikelsons C, Reid K, et al. Non-invasive ventilation in chronic obstructive pulmonary disease: management of acute type 2 respiratory failure. Clin Med (Lond). 2008;8(5):517-521.
doi - Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000;355(9219):1931-1935.
doi - Lote CJ. Renal regulation of body fluid pH. In: Principles of renal physiology. 4th edition; 2000. Kluwer Academic Publishers, Great Britain. ISBN: 978-0-7923-6178-7.
doi - Jonville S, Delpech N, Denjean A. Contribution of respiratory acidosis to diaphragmatic fatigue at exercise. Eur Respir J. 2002;19(6):1079-1086.
doi pubmed - Wood LDH. The Pathophysiology and Differential Diagnosis of Acute Respiratory Failure. In: Principles of Critical Care. 3rd edition, 2005. McGraw-Hill, USA. ISBN: 0-07-141640-4.
- Roberts CM, Stone RA, Buckingham RJ, Pursey NA, Lowe D. Acidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbations. Thorax. 2011;66(1):43-48.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








