| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 7, July 2016, pages 312-314
Gastric Bezoar Causing Massive Gastric Distention and Functional Outlet Obstruction in a Patient With Bulimia Nervosa
Richard M. Fazioa, c, Prasun Shahb, Eiei Soeb, Kadirawelpillai Iswarab, Ioana Chena
aDepartment of Internal Medicine, Maimonides Medical Center, Brooklyn, NY, USA
bDepartment of Gastroenterology, Maimonides Medical Center, Brooklyn, NY, USA
cCorresponding Author: Richard M. Fazio, Department of Internal Medicine, Maimonides Medical Center, 4802 Tenth Ave, Brooklyn, NY 11219, USA
Manuscript accepted for publication June 17, 2016
Short title: Gastric Bezoar in Bulimia Nervosa
doi: http://dx.doi.org/10.14740/jmc2560w
| Abstract | ▴Top |
Gastric bezoar is an uncommon cause of gastric outlet obstruction, as well as a rare complication of bulimia nervosa (BN). The authors report a case of a young female with a history of BN presenting with acute gastric outlet obstruction. Radiologic imaging revealed a markedly dilated stomach and a retained gastric bezoar was identified during endoscopy. She was treated conservatively with nasogastric intubation and fluid resuscitation, followed by the consumption of Coca-Cola® to promote fragmentation of the bezoar. The patient’s symptoms improved and she was transferred to a skilled eating disorder facility for further treatment of her underlying condition.
Keywords: Stomach; Gastric outlet obstruction; Bezoars; Bulimia nervosa
| Introduction | ▴Top |
Bulimia nervosa (BN) is a mental health disorder characterized by binge eating episodes, followed by purging techniques, in the form of self-induced vomiting, laxative abuse and off-label use of diuretics. Over time, many of these patients experience complications to the gastrointestinal system as caused by their repetitive habits. Formation of a gastric bezoar and subsequent functional gastric outlet obstruction is a rare complication of this disease and requires a high level of suspicion to prevent eventual mucosal ulceration, necrosis and even death in this subset of patients.
| Case Report | ▴Top |
A 21-year-old female presented to the emergency department (ED) with a 1-day history of abdominal pain, fullness, nausea and retching without vomiting. The pain was described as a constant sharp pain, located diffusely throughout the abdomen without radiation. Her last bowel movement was 2 days prior to presentation, with absence of flatus for 1 day. She denied fever, chills, chest pain and shortness of breath. The patient had a history of BN, diagnosed at the age of 14. She described a pattern of restrictive eating along with binge eating episodes and purging with induced vomiting and laxative use. Her last binge was approximately 12 h prior to arrival to ED, after which she had been unable to undergo self-induced vomiting. She was not able to quantify the amount of food consumed on a typical binge, but denied any consumption of non-food items including hair.
On admission, the patient was afebrile, normotensive with mild tachycardia (100 bpm) and saturating well on ambient air. The patient’s body mass index (BMI) was measured as 21.2 kg/m2. The abdomen appeared largely distended on inspection. A succussion splash was present on auscultation as well as high-pitched bowel sounds at rest. There was discernible tenderness to palpation most notable at the epigastrium, absent rebound tenderness and the liver and spleen were not palpable. Initial lab workup showed a white blood cell count of 9,400/UL, hemoglobin of 8.0 g/dL, hematocrit of 26.4% with a mean corpuscular volume of 74.2, and a platelet count of 301,000/UL. Basic metabolic panel did not indicate any electrolyte imbalance. The patient’s liver profile was found to be within normal limits and a TSH was mildly elevated at 5.52 mIU/L. Urine pregnancy test was negative. CT scan illustrated a markedly distended stomach (30.9 × 16.1 cm) with contained food matter (Figs. 1 and 2). A salem sump was inserted and placed to suction with immediate return of brown-colored stomach contents amounting to approximately 1.5 L. The patient underwent an esophagogastroduodenoscopy (EGD), which identified a large, linear appearing bezoar present in the greater curvature of the stomach and overlying the pylorus, without any signs of mucosal bleeding or necrosis (Fig. 3). The patient received Coca-Cola® by mouth to promote dissolution of the bezoar, along with metochlopramide for its promotility effects. Her diet was progressively advanced, as tolerated, and she was started on a more structured eating schedule centered on smaller, more frequent meals. Symptoms improved and she was transferred to a specialized eating disorder center for continued psychotherapy and nutritional support.
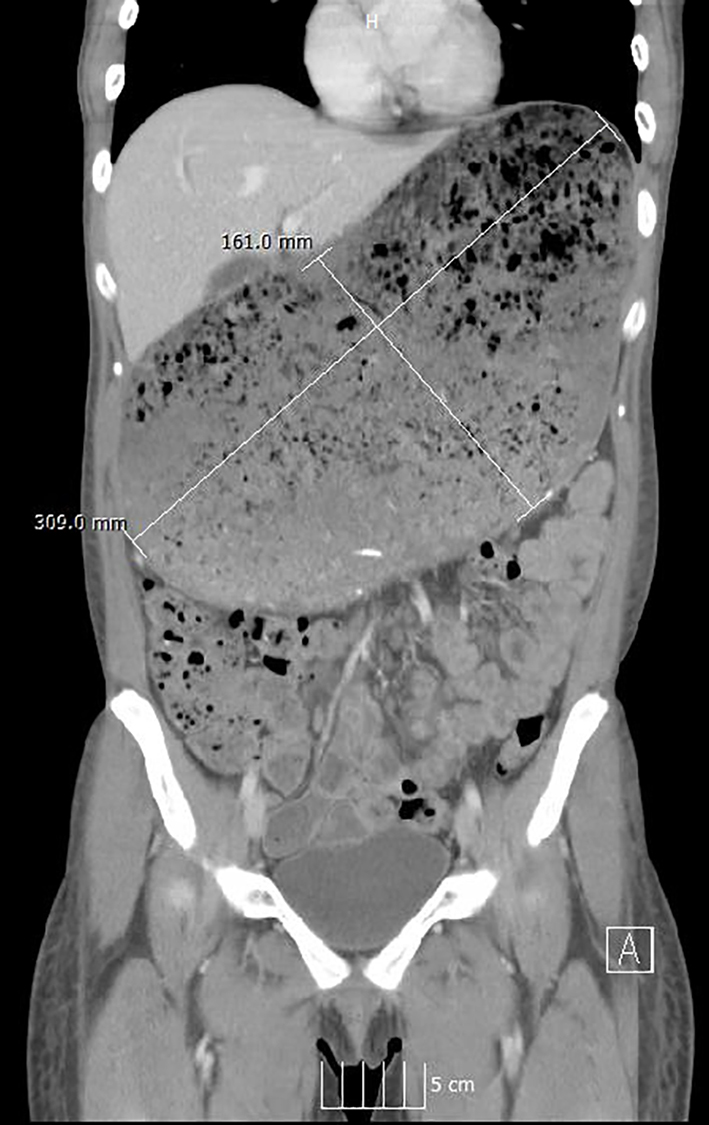 Click for large image | Figure 1. Coronal CT of the abdomen/pelvis displaying a massively distended stomach with retained food material, measuring at 30.9 × 16.1 cm in size. |
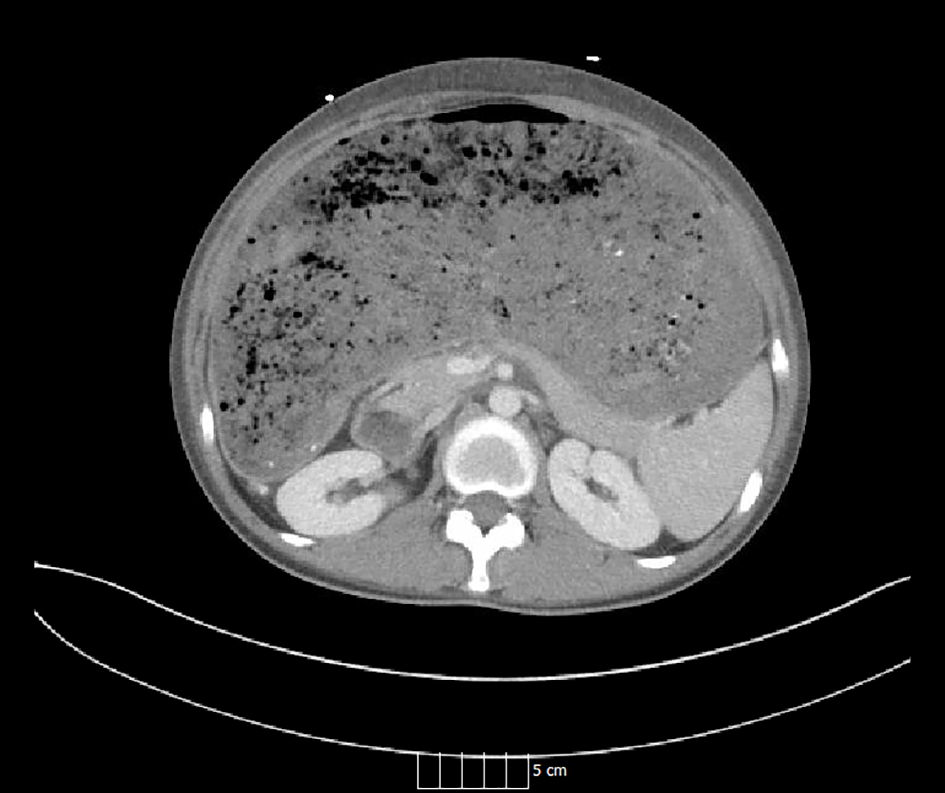 Click for large image | Figure 2. Axial CT of the abdomen illustrating a distended stomach. |
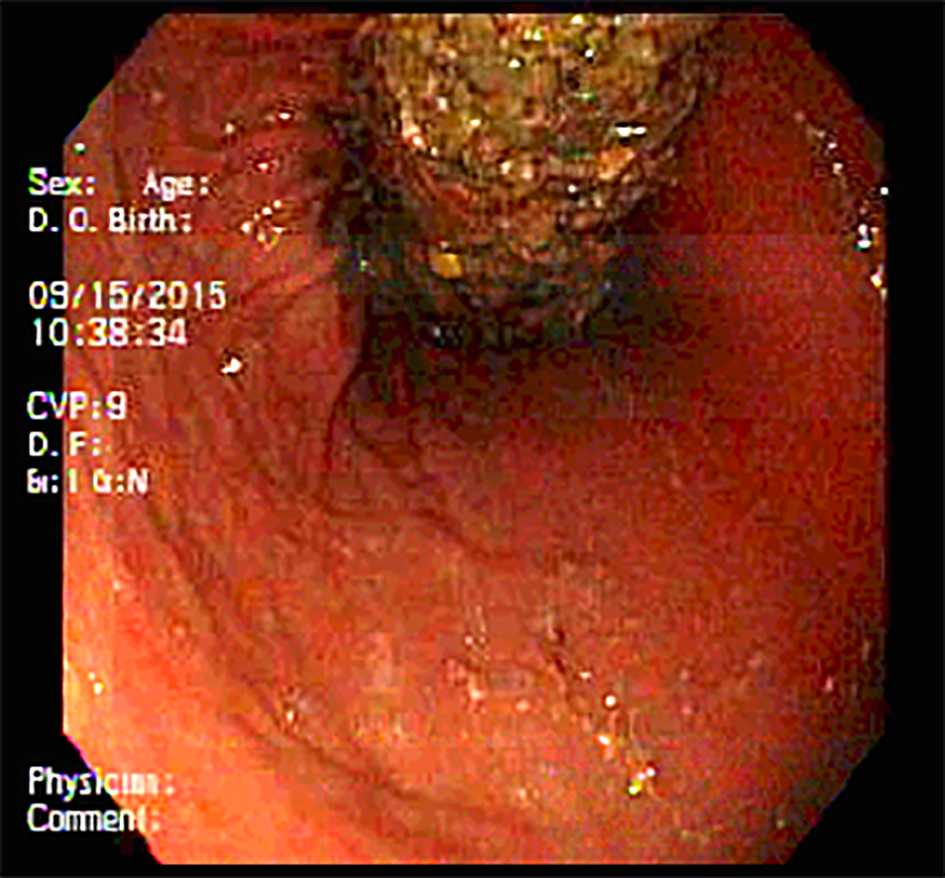 Click for large image | Figure 3. Endoscopic view of retained gastric bezoar. |
| Discussion | ▴Top |
BN is an eating disorder involving recurrent binge eating episodes, followed by inappropriate compensatory purging techniques (i.e., self-induced vomiting, overuse of laxatives and/or diuretics, excessive exercise, etc.). DSM-V diagnostic criteria include a lack of control during binge eating which consists of abnormally large portions of food, occurring at least once a week for three consecutive months, and associated with a fear of gaining weight and body dysmorphia. The disorder generally begins in adolescence and is predominantly identified in females as compared to males with a ratio of 10:1 [1, 2].
Patients may experience an array of self-imposed negative effects on the gastrointestinal tract, which can oftentimes be the presenting symptom of a patient’s underlying psychiatric disorder. Complications include gastroesophageal reflux disease and dyspepsia secondary to repetitive mucosal exposure to gastric contents, hematemesis and anemia caused by Mallory-Weiss tears, along with electrolyte disturbances related to gastric, colonic and renal losses [2, 3]. A gastric bezoar is a rare complication of BN [4]. It is described as an indigestible mass within the gastrointestinal tract, created by the coalesence of various materials, either intentionally or unintentionally. These materials may include the accumulation of fibrous fruit and vegetable material (i.e., phytobezoar), ingested hair (i.e., trichobezoar), medications (i.e., pharmacobezoar), retained milk products (i.e., lactobezoar) or even plastic and metal particles [5, 6]. Side effects of retained bezoars include ulceration of intraluminal mucosa with subsequent bleeding, along with gastric or small bowel obstruction and ileus, depending on its location. The formation of a gastric bezoar in this subset of patients is likely multifactorial, owing to an increase in gastric capacity, delayed gastric emptying, prolonged gastrointestinal transit time, abnormal autonomic functioning, impaired satiety thought to be secondary to decreased cholecystokinin release and the sheer size of meals consumed [7-9].
Management of a gastric bezoar consists of either a medical, endoscopic or surgical approach. Initial therapy consists of a dissolving agent in the form of cola, which, due to its acidity, carbonation and mucolytic properties, is able to promote the natural breakdown of the bezoar [10]. Promotility agents are used to improve gastric and intestinal peristalsis leading to the eventual advancement of fragmented food particles. Endoscopic tools in the form of forceps, snares, basket catheters and lithotripsy devices allow for mechanical fragmentation. Finally, in the event of continued symptoms or refractory bezoars, surgical removal would be indicated [2, 5]. In this particular patient, however, following stabilization and symptomatic improvement, the most important treatment consists of psychotherapy and nutritional support.
Conclusion
As opposed to a patient with anorexia nervosa who classically presents with an abnormally low BMI and lab values consistent with malnutrition, the diagnosis of BN may not be as apparent on initial presentation. Rather, in this subset of patients, BMI is typically within normal limits or even slightly elevated. Suspicion should be high when evaluating a young female presenting with gastrointestinal complaints, as the ultimate treatment for those suffering with BN comes with identification of their underlying disease.
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
| References | ▴Top |
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington, VA: American Psychiatric Publishing Co; 2013.
- Mehler PS. Clinical practice. Bulimia nervosa. N Engl J Med. 2003;349(9):875-881.
doi pubmed - Robinson PH. The Gatrointestinal Tract in Eating Disorders. Eur Eat Disorders Rev. 2000;8(2):88-97.
doi - Pedrolli C, Sacchi MC, Togni M, Cereda E. A case of hyperemesis in bulimia nervosa. Int J Eat Disord. 2015;48(4):446-448.
doi pubmed - Iwamuro M, Okada H, Matsueda K, Inaba T, Kusumoto C, Imagawa A, Yamamoto K. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc. 2015;7(4):336-345.
pubmed - Kumar GS, Amar V, Ramesh B, Abbey RK. Bizarre metal bezoar: a case report. Indian J Surg. 2013;75(Suppl 1):356-358.
doi pubmed - Stacher G. Gut function in anorexia nervosa and bulimia nervosa. Scand J Gastroenterol. 2003;38(6):573-587.
doi pubmed - Hadley SJ, Walsh BT. Gatrointestinal Disturbances in Anorexia Nervosa and Bulimia Nervosa. Curr Drug Targets CNS Neurol Disord. 2003;2(1):1-9.
doi - Geracioti TD, Jr., Liddle RA. Impaired cholecystokinin secretion in bulimia nervosa. N Engl J Med. 1988;319(11):683-688.
doi pubmed - Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis I. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther. 2013;37(2):169-173.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








