| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 11, November 2014, pages 601-602
Fetal Movements During Fetal Brain Death-Like Status
Shunji Suzukia, b, Kazuho Nakanishia, Aiko Yokoyamaa, Sakae Kumasakaa
aDepartment of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo, Japan
bCorresponding Author: Shunji Suzuki, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, 5-11-12 Tateishi, Katsushika-ku, Tokyo 124-0012, Japan
Manuscript accepted for publication October 13, 2014
Short title: Fetal Brain Death
doi: http://dx.doi.org/10.14740/jmc1974w
| Abstract | ▴Top |
The clinical features of fetal brain death syndrome include fixing of fetal heart rate (FHR) without decelerations and loss of fetal movements. Except the presence of fetal movements, the time course and outcomes of our current case are exactly the same as those in fetal brain death syndrome. A floppy female infant without detectable anomalies was delivered by cesarean section. The neonate weighed 2,782 g and Apgar scores were 0, 3 and 4 at 1, 5 and 10 minutes, respectively. An umbilical artery (UA) blood sample showed pH 7.373, PaCO2 37.5 mm Hg and base excess -3.0 mEq/L, respectively. The etiological mechanism leading to the fetal movements in the current case is not clear.
Keywords: Fetal brain death-like status; Syndrome; Fetal movements
| Introduction | ▴Top |
Fetal brain death syndrome has been thought to have similar characteristics to severe hypoxic-ischemic encephalopathy in utero [1]. The clinical features of fetal brain death syndrome include fixing of fetal heart rate (FHR) without decelerations and loss of fetal movements [1-6]. The etiological mechanism is thought to be chronic or acute hypoxia, resulting from a pathological state such as a temporary disruption of umbilical blood flow. However, it is unknown when the fetal brain damage occurs and how it progresses in fetal brain death syndrome. Recently, we have encountered a case of severe fetal brain damage, which is exactly the same as fetal brain death syndrome [1-6]. In the case with severe brain death-like status, however, fetal movements were observed until delivery.
| Case Report | ▴Top |
A 28-year-old woman, gravida 1 para 0, visited our hospital for her routine prenatal care at 38 weeks and 5 days of gestation. She felt a presence of fetal movements; however, the FHR showed a fixed pattern of 150 bpm without normal baseline variabilities, accelerations or decelerations, and it did not change during uterine contractions by routinely cardiotocograms. The result of vibroacoustic stimulation test (VAST) was negative; there was no change in FHR and movements under the vibroacoustic stimulation (Fig. 1). Sonographic examination revealed normal fetal growth and amniotic fluid volume. We measured peak systolic and end-diastolic velocity in the middle cerebral artery (MCA) and umbilical artery (UA). The resistance index (RI) of UA was normal (0.48); however, the MCA showed a high diastolic blood flow velocity and the RI was at an extremely low level of 0.47, indicating a brain-sparing effect. By ultrasonography, the presence of fetal breathing movements could not be recognized with certainty; however, the fetus was seemed to repeatedly sink in the amniotic cavity and to repeatedly rebound in the reaction of reaching the bottom of the amniotic cavity. The mother felt the fetal movements repeated regularly until delivery.
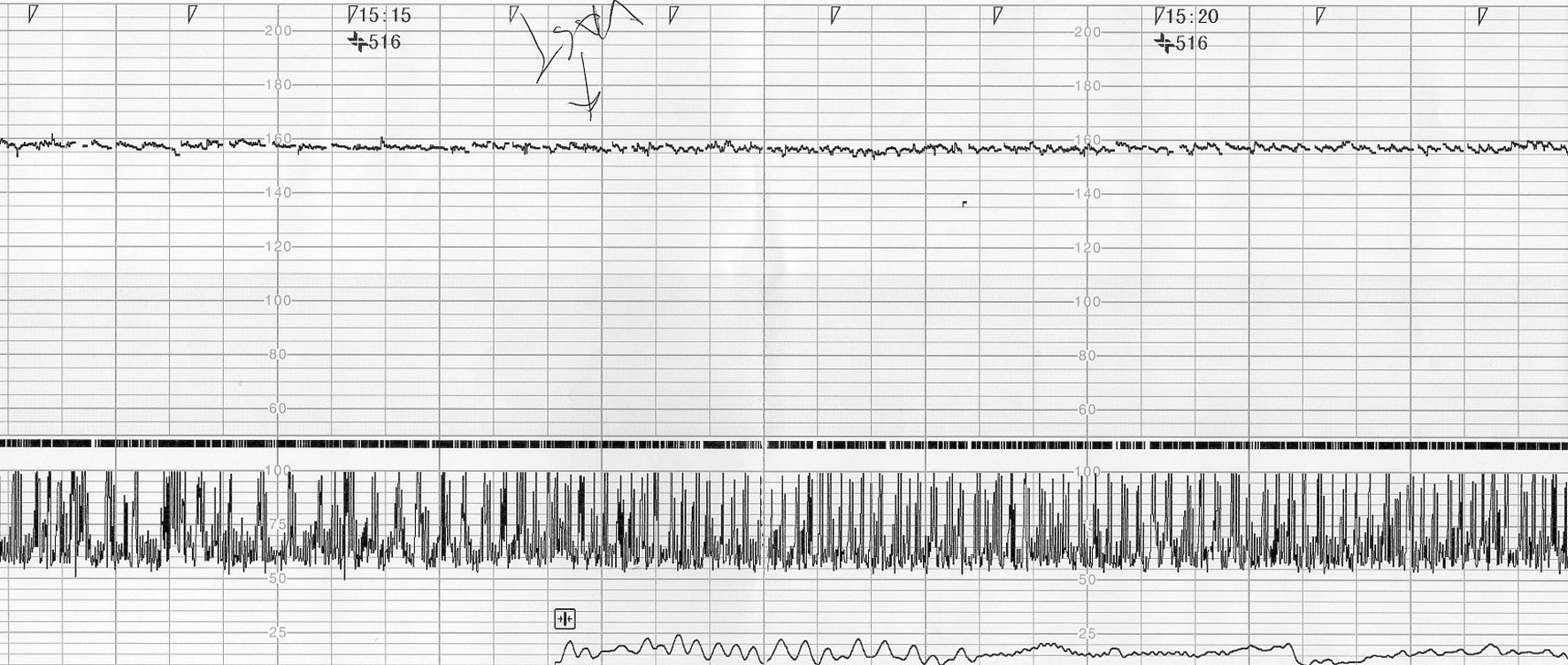 Figure 1. Fixed fetal heart rate pattern of 150 bpm with fetal movements. The result of vibroacoustic stimulation test was negative. Figure 1. Fixed fetal heart rate pattern of 150 bpm with fetal movements. The result of vibroacoustic stimulation test was negative. |
A floppy female infant without detectable anomalies was delivered by cesarean section based on an informed consent concerning the possibility of fetal brain death-like state [7]. The neonate weighed 2,782 g and Apgar scores were 0, 3 and 4 at 1, 5 and 10 min, respectively. The placenta and cord were normal. A UA blood sample showed pH 7.373, PaCO2 37.5 mm Hg and base excess -3.0 mEq/L, respectively. After endotracheal intubation and resuscitation, the infant was admitted to the neonatal intensive care unit. No spontaneous breathing or body movements, somatic or primitive reflexes, or pupillary light reflex were observed. At admission, a neonatal ultrasound examination showed that the RI was very low at 0.09 in the MCA (Fig. 2) and luxury perfusion continued. Her lactate dehydrogenase 943 IU/L and creatine kinase 199 U/L were not elevated. Electroencephalography was performed at 1 day of age and gave almost flat readings. A cerebral ultrasound examination at 8 days of age showed the presence of ventricular distention and cerebral atrophy. Therefore, the presence of severe intrauterine fetal brain damage was confirmed.
 Figure 2. Neonatal ultrasound examination showing the decreased resistance index of middle cerebral artery (0.09). Figure 2. Neonatal ultrasound examination showing the decreased resistance index of middle cerebral artery (0.09). |
| Discussion | ▴Top |
Except the presence of fetal movements, the time course and outcomes of our current case are exactly the same as those in fetal brain death syndrome reported previously [1-6]. The clinical features of fetal brain death syndrome include fixing of FHR and loss of any fetal movements. In the current case, however the fetus was seemed to repeatedly sink in the amniotic cavity and to repeatedly rebound in the reaction of reaching the bottom of the amniotic cavity. It was a simple and repeated movement looking like decerebrate and/or primitive reflexes. Unfortunately, we did not record the video of these fetal movements. The etiological mechanism leading to the fetal movements in the current case is not clear. We image that it is a little previous state of complete fetal brain death. To clarify the development of fetal brain death syndrome, the accumulation of similar case reports is needed.
| References | ▴Top |
- Nishimaki S, Iwasaki S, Miyamae T, Mori M, Yokota S. Cerebral blood flow in a case of fetal brain death syndrome. Ultrasound Obstet Gynecol. 2008;32(7):956-958.
doi pubmed - Chen YT, Hsu ST, Tseng JJ, Chen WC, Ho ES, Chou MM. Cardiotocographic and Doppler ultrasonographic findings in a fetus with brain death syndrome. Taiwan J Obstet Gynecol. 2006;45(3):279-282.
doi - James SJ. Fetal brain death syndrome--a case report and literature review. Aust N Z J Obstet Gynaecol. 1998;38(2):217-220.
doi pubmed - Nijhuis JG, Kruyt N, van Wijck JA. Fetal brain death. Two case reports. Br J Obstet Gynaecol. 1988;95(2):197-200.
doi pubmed - Nijhuis JG, Crevels AJ, van Dongen PW. Fetal brain death: the definition of a fetal heart rate pattern and its clinical consequences. Obstet Gynecol Surv. 1990;45(4):229-232.
doi pubmed - Zimmer EZ, Jakobi P, Goldstein I, Gutterman E. Cardiotocographic and sonographic findings in two cases of antenatally diagnosed intrauterine fetal brain death. Prenat Diagn. 1992;12(4):271-276.
doi pubmed - Ueda K, Ikeda T, Katsuragi S, Parer JT. Spontaneous in utero recovery of a fetus in a brain death-like state. J Obstet Gynaecol Res. 2010;36(2):393-396.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








