| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 2, February 2014, pages 113-115
Primary Angiosarcoma of Small Intestine Presenting With Intestinal Perforation: A Case Report
Ebru Zemheria, Pinar Engina, Seyma Ozkanlia, c, Ibrahim Ali Ozemirb
aDepartment of Pathology, Goztepe Training and Research Hospital, Istanbul Medeniyet University, Istanbul, Turkey
bDepartment of General Surgery, Goztepe Training and Research Hospital, Istanbul Medeniyet University, Istanbul, Turkey
cCorresponding author: Seyma Ozkanli, Tutuncu Mehmet EfendiCaddesi, KaranfilSokak, Ugur Apt. No:16/3 Goztepe-Istanbul, Turkiye
Manuscript accepted for publication January 14, 2014
Short title: Primary Angiosarcoma of Small Intestine
doi: https://doi.org/10.14740/jmc1653w
| Abstract | ▴Top |
Primary angiosarcomas are rare high-grade vascular tumors that mostly have poor prognosis. Angiosarcoma can resemble a gastrointestinal stromal tumor, leiomyosarcoma, a metastatic melanoma, a lymphoma, a poorly differentiated carcinoma, neuroendocrine tumor, or mesothelioma. On the other hand, the pathogenesis of an intestinal angiosarcoma is not clear and many etiologic factors have been suggested. In this report, we reviewed the English-written literature about primary intestinal angiosarcomas and analyzed a case of 78-year-old female patient with intestinal angiosarcoma presenting with intestinal perforation and acute abdomen.
Keywords: Primary angiosarcoma; Small intestine; Intestinal perforation
| Introduction | ▴Top |
Primary gastrointestinal angiosarcomas are very rare and angiosarcoma of small intestine is even rarer, with poor prognosis [1]. Angiosarcomas which account for only 1% to 2% of all soft tissue sarcomas are rare malignant tumors of endothelial origin [2]. These tumors have predilection for skin and superficial soft tissue, breast, bone, liver; they are rarely seen in deep soft tissue [3]. They are associated with chronic lymphedema, previous radiotherapy, and arteriovenous fistulas in renal transplant patients [1, 4]. In our case report, we present a 78-year-old woman presented with acute abdomen and intestinal perforation.
| Case Report | ▴Top |
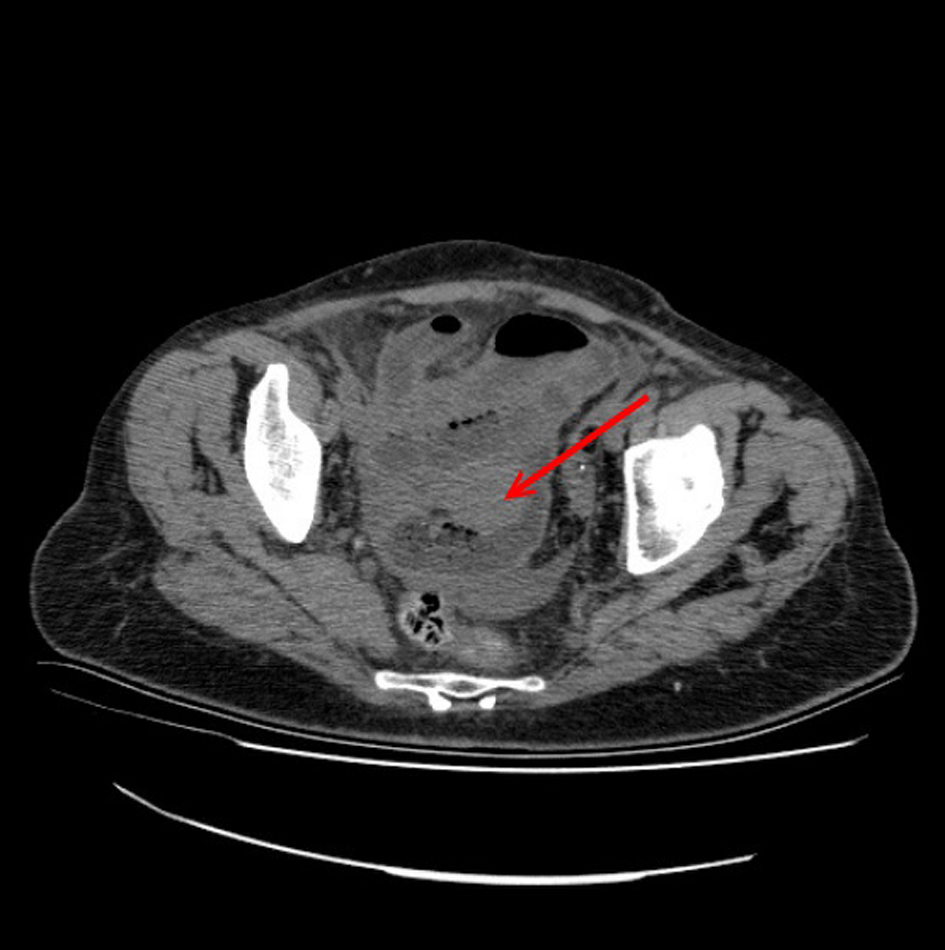
A 78-year-old woman with a known history of congestive heart failure, hypertension, and by-pass surgery was referred to our hospital’s emergency service with abdominal pain, nausea, vomiting, and constipation that continued for 2 days. She had pain in upper quadrant. On physical examination, there was tenderness in whole abdomen with rebound and guarding on the left side. There was no hepatomegaly or splenomegaly. Laboratory tests were performed; they showed leukocytosis, WBC: 11.8 × 103/µL (4.0 - 10.0) with neutrophilic predominance (89%), there was also anemia, RBC: 2.8 × 1012, Hb: 7.3g/dL (11.5 - 16), Hct: 22.4 (37-47%), thrombocytes were slightly higher than normal (541; N: 150 - 500). CRP was also higher than normal (38.4, N: 0 - 0.5). CT scans of abdomen revealed dilatation in intestinal loops (Fig. 1) and effusion in the abdomen (Fig. 2). She underwent a surgery due to acute abdomen.
 Click for large image | Figure 1. Axial sectional computed tomographic image shows dilated intestinal loops (arrow). |
 Click for large image | Figure 2. Cross sectional computed tomographic image shows a collection of free fluid in abdomen (arrow). |
At laparotomy, 1,000 mL seropurulent fluid was seen and aspirated; 90 cm distal to Treitz Ligament, a small perforation was detected at the serosal surface of jejunum. No other pathology was seen during laparotomy. A segment of 10 cm of small intestine and local mesentery of small intestine were resected. On macroscopic examination, serosa was covered with fibrinous material in one region, perforation was not seen grossly. Mucosal surface was edematous at most parts and hyperemic in the region where the serosal surface was covered with fibrinous material. On cut surface, there was a small white-tan colored nodule of 2 cm diameter that localized beneath the mucosa and extending to serosa.
On microscopic examination, tumoral nodules beneath the mucosa and serosa were seen (Fig. 3). Tumor cells were highly pleomorphic, epithelioid; arranged in solid aggregates, seemed to be related with large vessels (Fig. 4). The nuclei were prominent in most cells. Immunohistochemistry revealed tumor cells were diffusely positive for CD 31 (Fig. 5) and vimentin, focally positive for CD 34. They were negative for cytokeratin and HMBE-45, S-100.
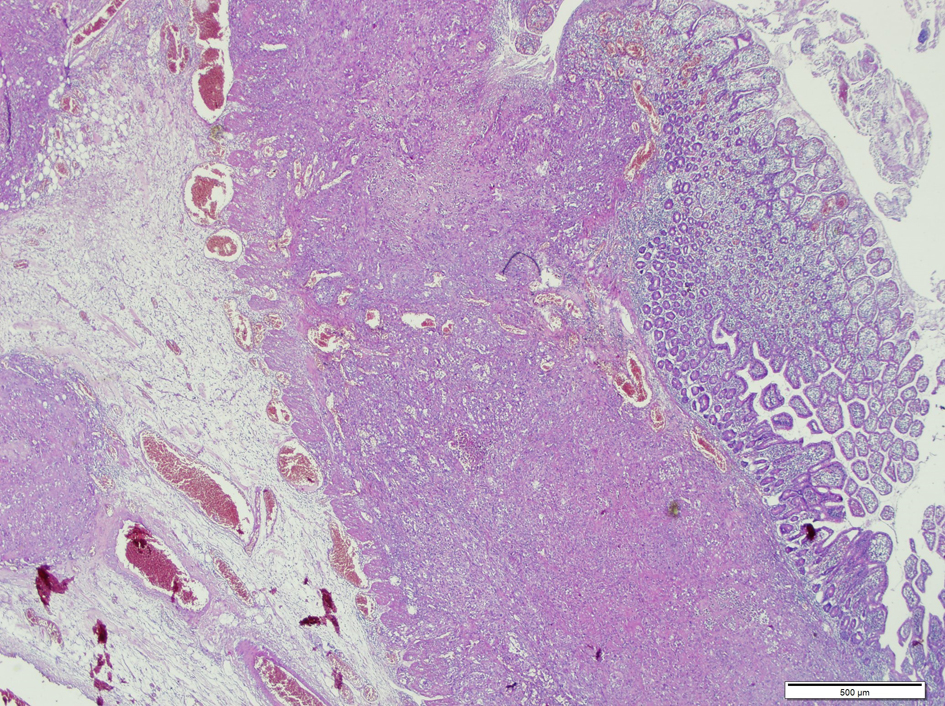 Click for large image | Figure 3. Tumoral foci beneath the mucosa and serosa (arrow) (hematoxylin-eosin). |
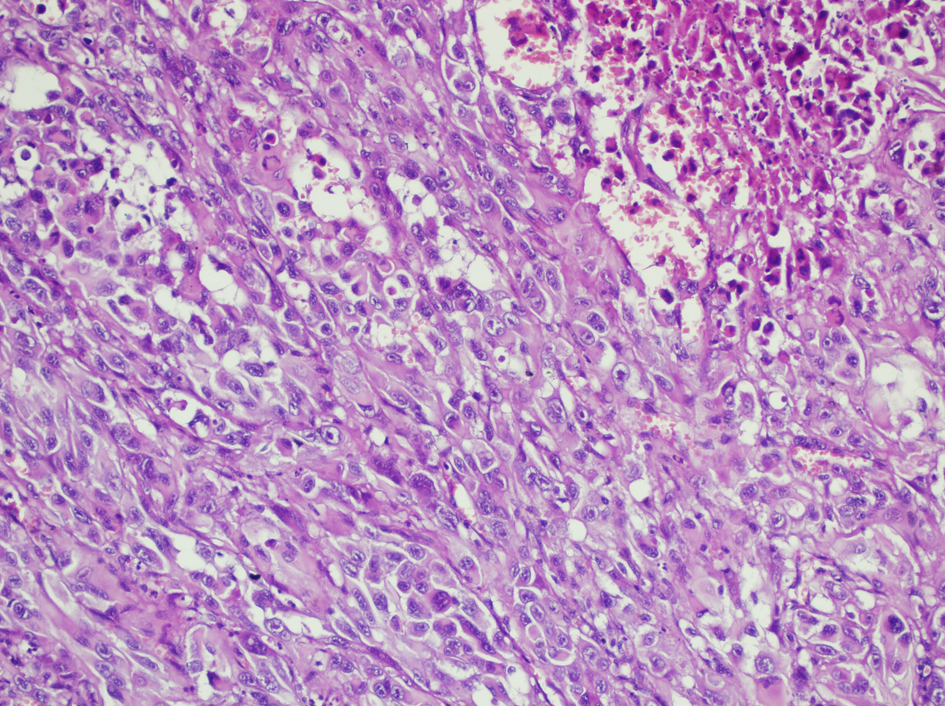 Click for large image | Figure 4. Tumor is composed of interlacing delicate vascular channels, solid sheets of spindle and undifferentiated cells, and erythrocytes (hematoxylin-eosin). |
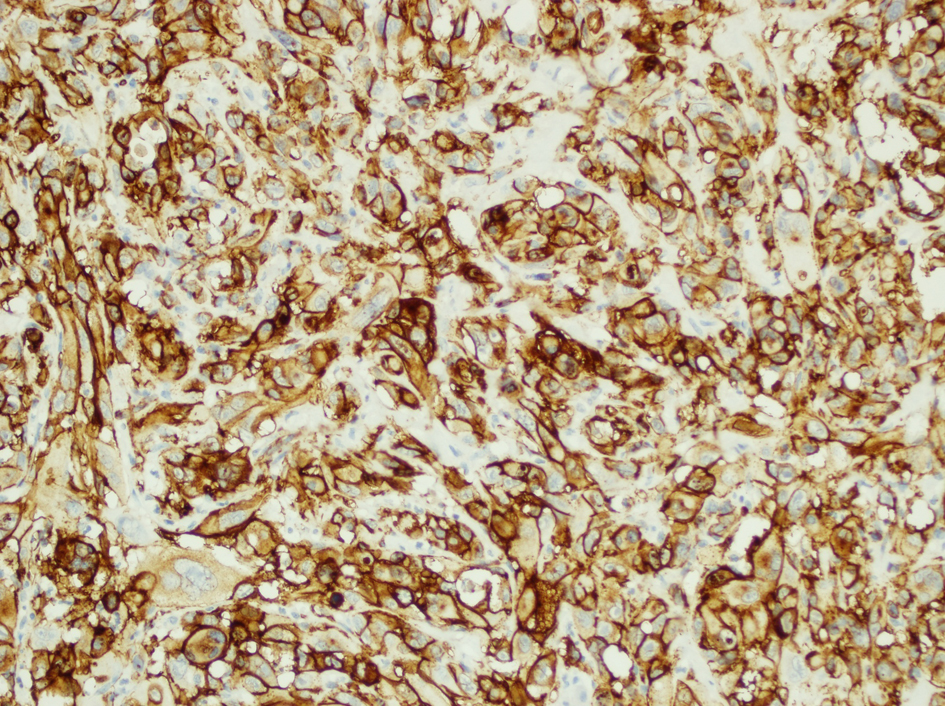 Click for large image | Figure 5. The tumor cells show strong positive staining with the endothelial marker, CD31 (Anti CD 31, × 20). |
| Discussion | ▴Top |
The three most frequent malignancies in the small intestine are neuroendocrine tumors, adenocarcinomas, and leiomyosarcomas [5]. Primary angiosarcomas of the small intestine are rare high grade vascular neoplasms [2]. Diagnosis is challenging due to non-specific clinical, radiological and histopathological findings [2].
The clinical findings of intestinal angiosarcoma are non-specific. Symptoms include abdominal pain, nausea, vomiting, intestinal obstruction, anemia, gastrointestinal bleeding [3, 6].
The pathogenesis of intestinal angiosarcoma is unclear; several etiologic factors have been suggested such as previous radiation, chronic lymphedema, exogenous toxins like thorotrast, vinyl chloride and arsenic, long-term peritoneal dialysis, intra-abdominal foreign body, visceral metastasis from Kaposi’s sarcoma and familial syndromes such as neurofibromatosis Type 1, mutated BRCA1 and BRCA2, Mafucci syndrome and Klippel-Trenaunay syndrome [1, 3, 4].
In the case report and review of the literature about primary angiosarcoma of the small intestine made by Qingqiang et al, they reported that 27 articles were found about angiosarcomas and only 21 of them were primary small intestinal angiosarcoma cases [1].
Magnetic resonance imaging (MRI), computerized tomography (CT), abdominal x-rays and ultrasound can be used for diagnosis but all of them have limited diagnostic utility [2, 7]. Conventional endoscopy is useful for tumors located in the stomach, duodenum and colon but not for jejunum and ileum. Although capsule endoscopy and barium can be used, they have limited diagnostic success [8]. Exploratory laparotomy is required for definitive diagnosis [3].
Our case report is intestinal angiosarcoma presenting with intestinal perforation and acute abdomen. Our patient had no history of etiologic factors. She had abdominal pain, nausea, vomiting, and constipation for two days. CT showed dilatation in intestinal loops and effusion in the abdomen. She underwent a surgery due to acute abdomen.
Angiosarcoma may be similar to a gastrointestinal stromal tumor, leiomyosarcoma, a metastatic melanoma, a lymphoma, a poorly differentiated carcinoma, neuroendocrine tumor, Crohnsdisease, mesothelioma [1, 2, 5, 9]. Microscopically anastomosing, delicate vascular channels lined by atypical endothelial cells mixed with solid sheets of spindled, epithelioid or undifferentiated cells are seen [2]. Cystic degeneration, cellular necrosis may be found [2]. Immunohistologically, intestinal angiosarcomas are positive for endothelial markers as CD31, CD34, von Willebrand factor, and vascular endothelial growth factor and negative for epithelial, neuronal and melanocytic markers as Keratins, S-100 and HMBE-45 [1, 2].
Conclusion
Angiosarcomas are rare tumors with poor prognosis; primary angiosarcomas of small intestine are even rarer with challenging clinical symptoms and diagnosis. They should be kept in mind that in differential diagnosis in cases presenting with intestinal perforation and acute abdomen especially if the patient is elderly and has anemia. A panel of immunohistochemical studies must be done to exclude other tumors and tumor-like lesions.
Conflict of Interests
We declare that there is no conflict of interests regarding the publication of this article and that we do not have a direct financial or personal relation with any people or organizations.
| References | ▴Top |
- Ni Q, Shang D, Peng H, Roy M, Liang G, Bi W, Gao X. Primary angiosarcoma of the small intestine with metastasis to the liver: a case report and review of the literature. World J Surg Oncol. 2013;11:242.
doi pubmed - Liu DS, Smith H, Lee MM, Djeric M. Small intestinal angiosarcoma masquerading as an appendiceal abscess. Ann R Coll Surg Engl. 2013;95(1):e22-24.
doi pubmed - Grewal JS, Daniel AR, Carson EJ, Catanzaro AT, Shehab TM, Tworek JA. Rapidly progressive metastatic multicentric epithelioid angiosarcoma of the small bowel: a case report and a review of literature. Int J Colorectal Dis. 2008;23(8):745-756.
doi pubmed - Khalil MF, Thomas A, Aassad A, Rubin M, Taub RN. Epithelioid Angiosarcoma of the Small Intestine After Occupational Exposure to Radiation and Polyvinyl Chloride: A case Report and Review of Literature. Sarcoma. 2005;9(3-4):161-164.
doi pubmed - Kelemen K, Yu QQ, Howard L. Small intestinal angiosarcoma leading to perforation and acute abdomen: a case report and review of the literature. Arch Pathol Lab Med. 2004;128(1):95-98.
pubmed - Mohammed A, Aliyu HO, Liman AA, Abdullahi K, Abubakar N. Angiosarcoma of the small intestine. Ann Afr Med. 2011;10(3):246-248.
doi pubmed - Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11(10):983-991.
doi - Knop FK, Hansen MB, Meisner S. Small-bowel hemangiosarcoma and capsule endoscopy. Endoscopy. 2003;35(7):637.
doi pubmed - Allison KH, Yoder BJ, Bronner MP, Goldblum JR, Rubin BP. Angiosarcoma involving the gastrointestinal tract: a series of primary and metastatic cases. Am J Surg Pathol. 2004;28(3):298-307.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








