| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 1, January 2014, pages 11-14
Surviving ARDS: A Case of Recurrent “Illicit Drug-Induced” ARDS
Nathan J. Smischneya, Kelly A. Cawcutta, Kannan Ramarb, Rahul Kashyapa, c
aDivision of Critical Care Medicine, Mayo Clinic, 200 First Street Southwest, Rochester, MN 55905, USA
bDivision of Pulmonary and Critical Care Medicine, Mayo Clinic, 200 First Street Southwest, Rochester, MN 55905, USA
cCorresponding author: Rahul Kashyap, Division of Critical Care Medicine, Mayo Clinic 200 First St SW, Rochester, MN 55905, USA
Manuscript accepted for publication November 8, 2013
Short title: Surviving Recurrent “Illicit Drug-Induced” ARDS
doi: https://doi.org/10.4021/jmc1571w
| Abstract | ▴Top |
Acute respiratory distress syndrome (ARDS) is a severe manifestation of abnormal pulmonary gas exchange. Many patients in whom this clinical syndrome develops are critically ill, and most do not recover. However, the critical care physician is likely to encounter more patients who have survived this clinical syndrome with recent improvements in the treatment related to this clinical entity. We describe a unique case of a patient who survived multiple episodes of ARDS. We illustrate potential etiologies relating to the multiple ARDS episodes and the recognition of illicit drug use as one of the pathophysiologic factors of recurrent ARDS. We highlight certain diagnostic clues in the patient’s history that may alert the intensivist to the diagnosis of ARDS related to illicit drug use.
Keywords: Acute respiratory distress syndrome; Crack cocaine; Heroin; Illicit drug; Intensive care unit; Recurrent; Surviving
| Introduction | ▴Top |
We discuss the first reported case of recurrent acute respiratory distress syndrome (ARDS) occurring more than two times in a patient. We describe the course of ARDS secondary to inhalational and intravenous (IV) illicit drug use, the surrounding differential diagnosis and what intensivists can learn from this unique case.
| Case Report | ▴Top |
A 37-year-old female with complete repair of tetralogy of Fallot as an infant and a current history of moderate to severe pulmonary regurgitation presented with acute hypoxic respiratory failure and ARDS requiring mechanical ventilation during most episodes in the setting of inhalational and IV illicit drug abuse. The diagnosis of ARDS was based on the 1994 American-European consensus conference definition [1] ratio of PaO2 to fraction of inspired oxygen (FIO2) (PaO2:FIO2), < 200; bilateral lung infiltrates present on chest radiograph (Fig. 1) and no clinical evidence of left atrial hypertension and was confirmed independently by two trained intensivists (N.S. and K.C.). We present a patient that developed ARDS five times over a 3.5-year period.
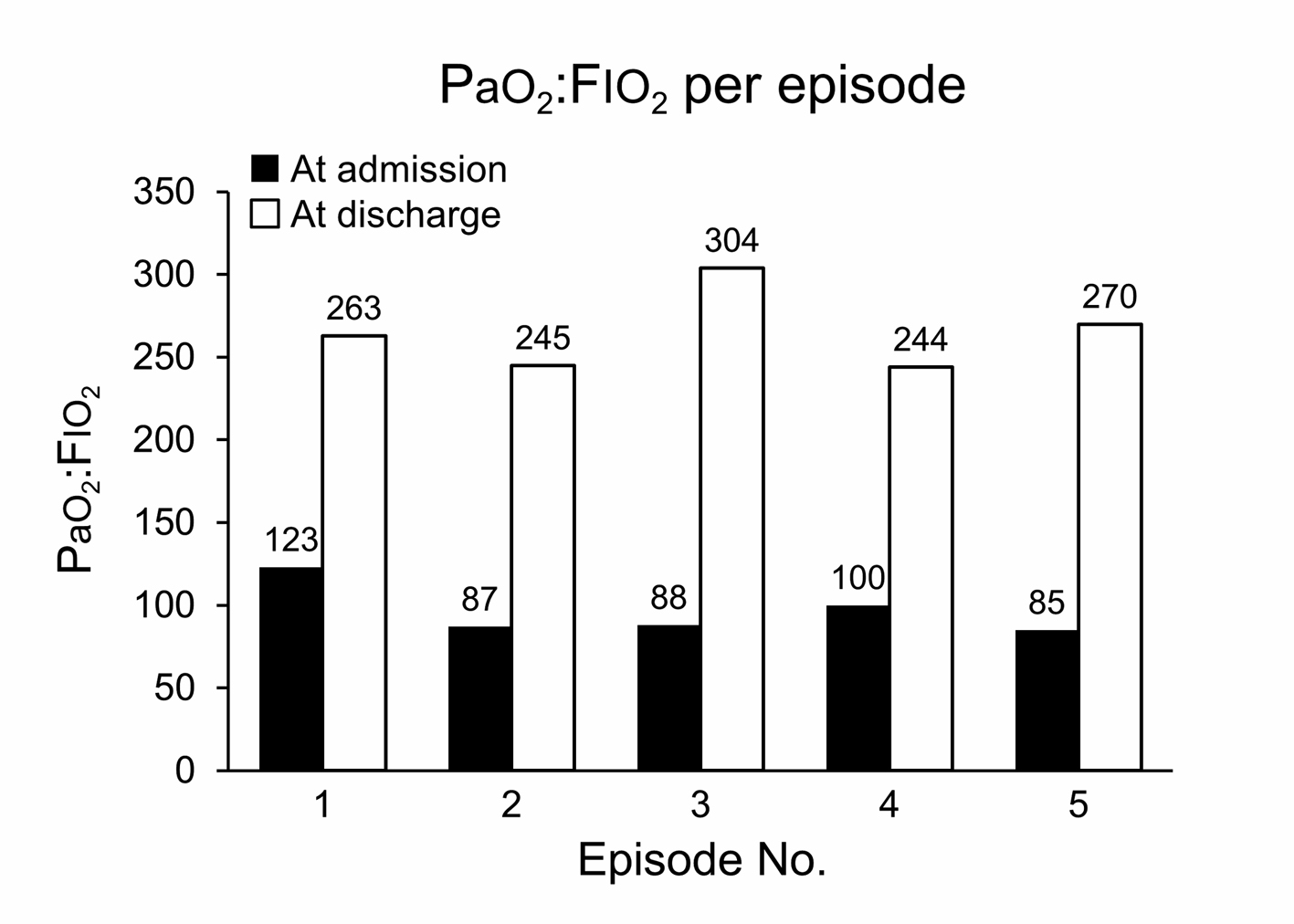 Click for large image | Figure 1. Ratio of PaO2 to fraction of inspired oxygen (FIO2) (PaO2:FIO2) with each episode of acute respiratory distress syndrome. |
First episode, April 2007
The patient presented to an Emergency Department (ED) with a 3 - 4 day history of productive cough, green-yellow sputum, shortness of breath and wheezing. She admitted to 5 - 7 days of continuous crack and IV heroin use. She was diagnosed as having crack lung with associated ARDS (PaO2:FIO2 = 123; chest X-ray findings: progression of diffuse bilateral pulmonary infiltrates), after exclusion of other etiologic factors. The patient recovered with empiric antibiotics and was liberated from mechanical ventilation after 20 days and discharged from the hospital shortly thereafter.
Second episode, March 2009
Two years later, the patient presented with shortness of breath, intermittent chills, fever, lower extremity swelling and was again admitted to the ICU. Her blood cultures were positive for methicillin resistant staphylococcus aureus and she was diagnosed with ARDS (PaO2:FIO2 = 87; chest X-ray findings: diffuse bilateral pulmonary infiltrates, most marked in the mid and lower lungs). She reported using heroin and crack on the day of admission and her urine toxicology screen was positive for cocaine. She received broad-spectrum antibiotics, required non-invasive mechanical ventilation for two days, and was discharged from the ICU within five days.
Third episode, May 2009
The patient presented to the ICU with complaints of worsening cough, dyspnea and some chills of several days duration. She was diagnosed with ARDS (PaO2:FIO2 = 88; chest X-ray findings: diffuse bilateral pulmonary infiltrates, most marked in the mid and lower lungs, new since last image). Her urine toxicology screen for illicit substances was negative and the cause of ARDS was attributed to either aspiration pneumonitis or substance abuse. Empiric antibiotics, steroids and diuresis were initiated. She was mechanically ventilated for six days, recovered and was discharged from the ICU on seventh day.
Fourth episode, October 2009
The patient presented with increasing shortness of breath of three days duration. She again admitted to having inhaled crack cocaine and used IV heroin on the day of admission. The diagnosis was ARDS, possibly due to either aspiration or heroin/crack toxicity (PaO2:FIO2 = 100; chest X-ray findings: alveolar infiltrates have developed throughout both lungs, greatest in the right mid and right lower lung). She was given broad-spectrum antibiotics and required closed faced mask for respiratory support. She recovered within five days and was discharged.
Fifth episode, August 2010
For this episode, the patient presented to an outside ED in acute respiratory distress, cyanotic and wheezing. She was intubated and placed on broad-spectrum antibiotics. She was diagnosed with ARDS related to substance abuse, which was confirmed through a positive urine toxicology screen (PaO2:FIO2 = 85; chest X-ray findings: diffuse bilateral pulmonary infiltrates are slightly more prominent since November 2009). She was mechanically ventilated for seven days and was discharged from the ICU on the eighth day.
The patient consistently met criteria for ARDS as per the 1994 American-European consensus conference definition [1] for all five admissions and met new ARDS criteria “Berlin Definition” [2] in all but one admission. For the four admissions in which she required mechanical ventilation the parameters were as follows: tidal volume of 330 - 550 mL, positive end-expiratory pressure of 7.5 - 13 cmH2O, plateau pressure of 32 - 39 cmH2O and FIO2 of 0.6-1.0. The patient had pulmonary function testing (PFT) performed on two occasions, one after the first episode and the other after the fourth episode. The first forced expiratory volume in 1 sec was 2.43 L, with no significant decline in the subsequent PFT (2.36 L), with the remainder unremarkable. The patient did not require supplemental oxygen at home between any of the ARDS episodes.
Through multiple admissions spanning 3.5 years, the evaluation of the etiologic factors for the patient’s recurrent hypoxic respiratory failure and ARDS centered on excluding possible congestive heart failure and pulmonary infection. Congestive heart failure was excluded on the basis of negative clinical examination findings, normal results on echocardiography (namely, ejection fraction > 50%, no new valvular lesions and stable pulmonary regurgitation) and normal levels of serum N-terminal pro-brain natriuretic peptide.
Given the appearance of infiltrates on chest imaging, the patient’s medical history of 3 - 5 days of self-reported cough, dyspnea and sputum production raised the concern for an infectious process and was among the leading differential diagnoses. However, bronchoscopy with lavage, cultures and laboratory data were negative for an infectious cause. Ultimately, since neither congestive heart failure nor an infectious cause was apparent and the patient had rapid clinical improvement, it was determined that the underlying cause of her ARDS was secondary to IV heroin and inhaled crack cocaine use.
| Discussion | ▴Top |
Recurrent ARDS of more than two episodes is rare. In this review, we determined that an inter-episode duration of less than 90 days is also a unique characteristic of this case. Similarly, the rapid improvement with no serious overall sequelae is unique and may be related to the underlying cause of ARDS (namely, illicit drug use in four incidents) in this patient.
Multiple known causes of initial episodes of ARDS include sepsis, trauma, gastric aspiration and the use of particular drugs (namely salicylates, heroin, methadone, lidocaine and propoxyphene) [3]. Recurrent respiratory failure of more than two episodes has rarely been reported, and the underlying causes in these cases have been secondary to aspirin use, propylthiouracil use or ketoacidosis [4]. The diagnosis of ARDS secondary to IV heroin and inhaled crack cocaine use is consistent with the relatively rapid clearance (< 7 days) of the patient’s infiltrates on four of the five admissions. Such rapid clearance of bilateral areas of increased opacities is characteristic of heroin-induced acute lung injury [5]. When heroin has been crushed or manipulated and taken via IV administration, microemboli can form and cause damage through inflammatory mediators. This effect is not unique to heroin; drug users crush various oral medications to be injected via the IV route.
Oral medications that are crushed and injected can have numerous consequences on the lung parenchyma because of multiple localized processes. The filler materials in oral medications may cause drug-induced pulmonary damage. Talc is an insoluble filler material that may result in occlusion of small vessels in the lungs because talc particles are embolized when injected. This occlusion can result in pulmonary hypertension leading to pulmonary edema and cause findings similar to those of our patient. On imaging, the talc particles appear as irregular nodular areas of increased opacity in the middle and upper lobes [5] (Fig. 2). Cellulose is another filler material that may be found when an oral substance has been crushed and injected. Cellulose is reported to cause numerous small nodules in the lungs, often in a centrilobular pattern [5].
 Click for large image | Figure 2. Chest radiographic image representative of heroin-induced acute respiratory distress syndrome during the patient’s fifth episode of ARDS. AP indicates anteroposterior; L, left; R, right. |
The prognosis for ARDS has improved markedly in recent years, with substantial reductions in reported mortality rates for single episodes of ARDS. Recurrent episodes have been noted to have an increased mortality rate compared with single episodes [6]. With improved survival in initial episodes of ARDS, recurrent episodes may become more common and may be subject to the same risk factors that predisposed a patient to the initial episode [4, 6]. Of note, although an underlying cause was discovered for the present patient, recurrent ARDS may be secondary to a new risk factor or insult or may continue to have no identifiable trigger.
Finally, the short inter-episode duration of our patient has not been reported previously. In fact, the median time between first and second episodes is documented as 264 days [6, 7]. Among the cases from which this median was derived, the median survival time after the second episode was only 22 days [6]. Our patient has survived, to date, a total of five admissions with recurrent ARDS.
For the intensivists, recognizing the possibility of recurrent ARDS is imperative to clinical care. With improved survival of initial episodes of ARDS, the probability of recurrent ARDS may be increased. A thorough medical history from the patient or the patient’s family must be obtained to assist with determination of the underlying cause. Drug-induced acute lung injury may be a unique risk factor for recurrence of ARDS and must be obtained in the history, especially in patients with mid-upper lobe involvement on imaging.
Summary
Because the recurrence of ARDS is rare, a clinician needs to consider the possibility of repeated exposure to toxins, infections or illicit drugs.
Recognize the importance in taking a complete history and physical including illicit drug use in all patients, especially with bilateral lung infiltrates.
Recurrent ARDS presenting with a predominant mid to upper lobe reticular nodular infiltrate on chest imaging that rapidly clears with minimal health sequel should raise the possibility of illicit drug use as the cause.
Conflict of Interest
None.
Financial Support
None.
Abbreviations
ARDS: acute respiratory distress syndrome; FIO2: fraction of inspired oxygen; ICU: intensive care unit; IV: intravenous; PFT: pulmonary function testing
| References | ▴Top |
- Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M,
et al . The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818-824.
doi pubmed - Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L,
et al . Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526-2533.
doi pubmed - Gonzolez ER, Cole T, Grimes MM, Fink RA, Fowler AA
3rd . Recurrent ARDS in a 39-year-old woman with migraine headaches. Chest. 1998;114(3):919-922.
doi pubmed - Savici D, Katzenstein AL. Diffuse alveolar damage and recurrent respiratory failure: report of 6 cases. Hum Pathol. 2001;32(12):1398-1402.
doi pubmed - Gotway MB, Marder SR, Hanks DK, Leung JW, Dawn SK, Gean AD, Reddy GP,
et al . Thoracic complications of illicit drug use: an organ system approach. Radiographics. 2002;22 Spec No:S119-135. - Bice T, Li G, Malinchoc M, Lee AS, Gajic O. Incidence and risk factors of recurrent acute lung injury. Crit Care Med. 2011;39(5):1069-1073.
doi pubmed - Kishimoto T, Ohke M, Ozaki S, Fujioka H, Kimura K, Sunami K, Yonei T,
et al . [Recurrence of the acute respiratory distress syndrome in a patient with liver cirrhosis and diabetes mellitus]. Nihon Kyobu Shikkan Gakkai Zasshi. 1996;34(5):586-591.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








