| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 4, April 2013, pages 201-203
Pelvic Fracture in the Pregnant Patient
Andrew L. Atkinsona, b, Douglas Sherlocka, Charles Huxa
aDepartment of Obstetrics and Gynecology, Jersey Shore University Medical Center, Neptune New Jersey, USA
bCorresponding author: Andrew L. Atkinson, 1945 Route 33, Neptune, NJ. 07753, USA
Manuscript accepted for publication January 2, 2013
Short title: Pelvic Fracture
doi: https://doi.org/10.4021/jmc1006w
| Abstract | ▴Top |
Pelvic fracture in the pregnant patient is a very rare occurrence that has very scant results on a medical literature search. We present a 33-year-old who was 20 weeks pregnant at the time of car accident that along with traumatic rupture of membranes also suffered an open book fracture of the pelvis. Management in coordination with obstetrics as well as the orthopedic team, the patient underwent an external fixation which allowed for induction of labor to deliver the non viable fetus. Once stable after delivery, an internal fixation was done and patient went on to make a full recovery.
Keywords: Pelvic fracture; Pregnant; Rupture of membranes
| Introduction | ▴Top |
Pelvic fracture in the pregnant and non pregnant patient alike is a serious life threatening injury that requires immediate attention as well as intervention to ensure a positive outcome. In the initial period of stabilization of the patient with a pelvic fracture, hemorrhage should always be on the mind of the caregiver. If hemorrhage should occur, blood pooling will most likely be found in the retroperitoneal space with imaging. The retroperitoneal space in the adult patient can hold up to 4 liters of blood. In the pregnant patient with hemorrhage, fetal hypoxia and risk of intrauterine fetal death rises substantially in the unstable patient. Rocking the pelvis should never be included in the physical exam if a fracture is suspected; this maneuver can displace the pelvis even further causing disruption of a stable hematoma causing more hemorrhage to occur. Injuries to other organs from fragments of dislocated, fractured bone should be high on the list in the evaluation of the injured pelvis. Trauma to the gravid uterus could compromise the pregnancy as well as cause physical damage to the fetus. Bladder neck as well as urethral injury is also a common occurrence with genitourinary injuries being found in up to 25% of pelvic fractures [1]. In the pregnant patient the gravid uterus will anteriorly displace the bladder moving it slowly out of the pelvis and into the abdomen making it more vulnerable to blunt or penetrating trauma. As described, multisystem assessment in the patient with pelvic fracture is a must to properly treat these patients. In the pregnant patient with pelvic fracture, knowledge of anatomical as well as physiologic changes that occur in the pregnancy is needed to maximize the best outcome for the fetus and the mother.
| Case Report | ▴Top |
We present a 33-year-old female whom presented via ambulance to the trauma bay after experiencing a head on collision on a local roadway. The patient was driving 55 mph and hit a vehicle on the driver’s side door of a SUV who had run a red light on a major crossway approximately 5 miles from the hospital. The patient was not wearing a seatbelt, and airbags were deployed.
At the time of motor vehicle accident, the patient was 20 weeks and 2 days pregnant. Her pregnancy had been uncomplicated thus far, and she had received adequate prenatal care up to that point. In the trauma bay, the patient reported that there had been a gush of fluid upon impact between her legs and it was observed that she was non ambulatory at the scene. Extensive bruising of the abdomen was noted on initial encounter in the trauma bay on arrival to the hospital. The patient was evaluated with a bedside ultrasound showing positive fetal cardiac activity, but scant fluid around the fetus with an amniotic fluid index of 3. A speculum exam was not able to be performed because of severe pain in relation to movement of her lower extremities. Clear fluid however was identified on the hospital bed and was found to be both nitrazine positive and have classic ferning pattern on microscopy. Further exam demonstrated adequate peripheral pulses with severe pain on palpation of her groin as well as pelvic region. Vitals were stable throughout the initial evaluation period in the trauma bay. The patient was eventually transported to radiology for imaging studies; it was found that the patient had a left symphysis pubis and right sacral ala to foramina fracture (Fig. 1). The patient had an open book pelvic fracture with her sacroiliac joint remaining supported by the posterior ligaments and causing her pelvis to open like a hinge, creating a pelvis that is vertically stable but rotationally unstable [2].
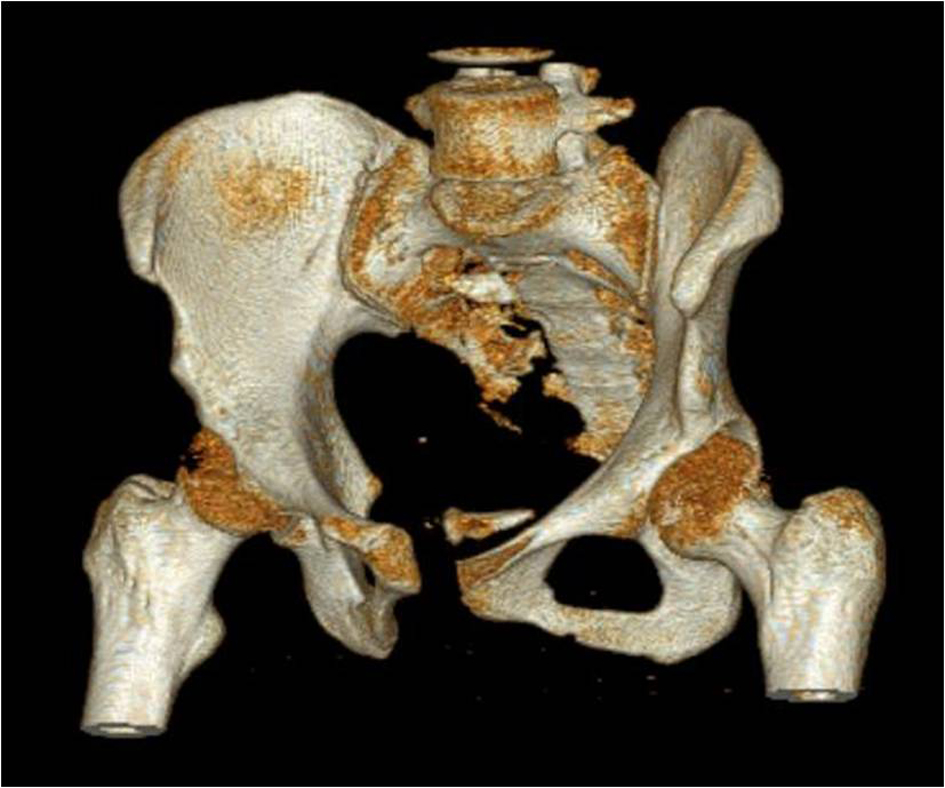 Click for large image | Figure 1. Three dimensional view of patients’ pelvic fracture. Notice the separation at the Pubis with a floating piece of bone within the pelvic brim. |
The patient and her family were counseled on the prognosis of the pregnancy and challenge of management with her orthopedic injuries. The infant’s gestational age had been previously confirmed with a first trimester ultrasound and was therefore confirmed nonviable at that time (on ultrasound there was no evidence of fetal trauma). The family understood the risk of continuing the pregnancy and agreed to undergo delivery of the nonviable fetus.
The patient was placed in a pelvic binder and underwent an anterior pelvic external fixation on hospital day number two. After the fixation procedure, the patient was able to sit up in bed and flex her hips 90 degrees. In coordination with Obstetrics as well as the Orthopedics physicians, it was determined that it was safe and feasible for the patient to undergo a vaginal delivery. Three doses of misoprostol 400 µg vaginally were used for induction of labor. She went on to deliver a stillborn male infant (no physical trauma noted) weighing 330 g, with minimal effort or strain on the mother’s part. The placenta however was retained after the fetal birth. A dose of 200 µg of misoprostol as well as carboprost 200 µg was also given in attempt to expel the retained placenta. Despite medications administered, the placenta remained retained for more than 3 hours. The patient was taken to the operating room where suction dilation and curettage was preformed under ultrasound guidance with an estimated blood loss of 900 milliliters. Postoperatively a complete blood count was done and patient hemoglobin was found to be 6.2, and hematocrit of 18.7. Two units of packed red blood cells were transfused immediately. Patient was stable after delivery and blood levels remained stable after transfusion. On hospital day eight, internal fixation, open reduction was performed. The Patient tolerated procedure well and had an unremarkable postoperative course. On hospital day number thirteen, patient was discharged to a rehabilitation facility. At 6 month follow up, she was walking unassisted with no abnormalities in her gait, the only complaint she had was dyspareunia.
| Discussion | ▴Top |
We describe a rare case of open book pelvic fracture in a pregnant woman. On a literature search using PubMed as well as Ovid, using search terms, “Pelvic Fracture”, “Pregnant” and “Traumatic Rupture of Membranes” identified one other case in published medical literature.
Pelvic fractures in pregnant patients are associated with a 9% maternal and a 35% fetal mortality rate, regardless of the type of fracture or the trimester of pregnancy [3]. However, fracture type (acetabular versus pelvic), and fracture designation (simple versus complex) had no influence on maternal or fetal mortality [4]. Automobile accidents affect up to 7% of pregnancies and account for the majority of pelvic and acetabular fractures occurring during pregnancy [5]. In our particular patient, the non viability status (< 24 weeks), as well as traumatically rupturing her membranes made the decision for termination of the pregnancy relatively straight forward. In dealing with viable infants the recommended method of delivery for pelvic and acetabular fractures during pregnancy depends on the presence or absence of initial fetal or maternal distress. Emergent cesarean delivery should be performed only for non-reassuring fetal status in these cases. The degree of fetal maturity, estimated gestational weight at the time of injury, severity of maternal injury, displacement of the pelvic or acetabular fracture, how recently the fracture occurred, are all factors that should be included in deciding whether to do a cesarean versus vaginal delivery in the stable patient with a pelvic fracture [6]. Standard pelvic fractures heal within 8 to 12 weeks; vaginal delivery should not be contraindicated after fractures have occurred in the early pregnancy period [4]. This case is a demonstration of the ability of an interdisciplinary team to facilitate standard obstetric management in a patient with open book pelvic fracture.
Disclosure
The authors report no conflict of interest. Written permission has been obtained from the patient to write this report. This Report has never been published in any other journal.
| References | ▴Top |
- Gibbs MA, Bosse MJ. Pelvic ring fractures. In: Ferrera PC, Colucciello SA, Marx JA, Verdile VP, Gibbs MA, eds. Trauma Management: An Emergency Medicine Approach. St Louis, Mo: Mosby; 1998:330-333.
- Tile M, ed. Fractures of the Pelvis and Acetabulum. 2nd ed. Baltimore, Md: Williams & Wilkins: 1995:41-52.
- Fildes J, Reed L, Jones N, Martin M, Barrett J. Trauma: the leading cause of maternal death. J Trauma. 1992;32(5):643-645.
doi pubmed - Leggon RE, Wood GC, Indeck MC. Pelvic fractures in pregnancy: factors influencing maternal and fetal outcomes. J Trauma. 2002;53(4):796-804.
doi pubmed - Occelli B, Depret-Mosser S, Renault B, Therby D, Codaccioni X, Monnier JC. [Pelvic trauma and pregnancy. Literature review and case report]. Contracept Fertil Sex. 1998;26(12):869-875.
pubmed - Morris JA, Jr., Rosenbower TJ, Jurkovich GJ, Hoyt DB, Harviel JD, Knudson MM, Miller RS, et al. Infant survival after cesarean section for trauma. Ann Surg. 1996;223(5):481-488; discussion 488-491.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








