| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 4, April 2013, pages 215-217
A Case of Trisomy 9 Complicated With Congenital Diaphragmatic Hernia
Takehiro Serikawaa, c, Keisuke Hondab, Mina Itsukaichia, Kyoko Yamadaa, Koichi Takakuwaa
aPerinatal Intensive Care Center, Niigata University Medical and Dental Hospital, Niigata, Japan
bDepartment of Obstetrics and Gynecology, Nagaoka Chuo General Hospital, Nagaoka, Japan
cCorresponding author: Takehiro Serikawa, Department of Obstetrics and Gynecology, Niigata University, 1-757 Asahimachi-dori, Chuoku, Niigata, 951-8510, Japan
Manuscript accepted for publication January 2, 2013
Short title: Trisomy 9
doi: https://doi.org/10.4021/jmc1003w
| Abstract | ▴Top |
We experienced a case with fetal trisomy 9, which was confirmed by genetic amniocentesis at the 28th week of gestation. A pregnancy woman of the 24th week of gestation with congenital diaphragmatic hernia (CDH) and intrauterine growth restriction (IUGR) was referred to our hospital. Magnetic resonance imaging (MRI) scans further depicted the detailed anatomical configurations of congenital diaphragmatic hernia, hydrops fetalis, agenesis of corps callosum, and cerebellar hypoplasia. Genetic amniocentesis revealed trisomy 9, a karyotype of 47, XY, +9 in the cultured amniocytes. At the 32nd week of gestation, intrauterine fetal death was confirmed and a stillborn male infant was delivered with a body weight of 875 g and a length of 39 cm after induction of labor. Macroscopic findings included small palpebral fissures, hypertelorism, micrognathia, low-set ears, hypoplastic phalanges, cryptorchidism, hypoplastic scrotum, micropenis, and rocker-bottom feet.
Keywords: Trisomy 9; Congenital diaphragmatic hernia; IUGR
| Introduction | ▴Top |
Fetal trisomy 9 is a relatively uncommon chromosomal abnormality that was first described by Feingold and Atkins in 1973 [1]. Various abnormalities are found that the characteristic facial changes include microphthalmia, deep-set ears, ear anomalies, micrognathia, large anterior fontanels, and bulbous nose. This condition is rare, accounting for only 1% of all chromosomally abnormal cases or 2.4% of trisomic cases among spontaneous abortions.
CDH is associated with chromosomal anomaly. The association of CDH with chromosomal anomalies such as trisomy 13 and 18 is well known [2]. The cases complicated with CDH associated with trisomy 9 have been reported by various countries [3-5]. In this report, we present a case of trisomy 9 associated with CDH and severe IUGR. The clinical course of the case would suggest the importance of correct diagnosis and appropriate patient counseling without delay. In addition, there are no English literatures about CDH associated with trisomy 9 and this case may be the first report in Japan.
| Case Report | ▴Top |
A 36-year-old Japanese pregnant woman (gravida 2, para 2) had been undergone prenatal managemen and care at the hospital near her residence. Fetal growth restriction had been pointed out since the 16th week of gestation and CDH was pointed out in the 24th week of gestation, so that this patient was referred to the obstetric outpatient clinic at Niigata University Medical and Dental Hospital for close examination of CDH and IUGR in the 25th week of gestation. Her obstetric, medical, and family histories were unremarkable. Her husband was 36 years of age and healthy. She and her husband were not consanguineous.
Ultrasonographic examinations performed at the first visit revealed left-side diaphragmatic hernia at our hospital (Fig. 1). Fetal lung area to head circumference was 0.83, below 1.0, so that severe lung hypoplasia was suspected. The estimated fetal weight was 385 g, corresponding to the 21st week of gestation, so that severe IUGR was suspected. Ventriculomegaly and narrowing of cysterna magna were also observed (Fig. 2). The amniotic fluid volume was within normal limits. She was hospitalized for close examination. Fetal MRI revealed CDH, no detection of left lung, hydrops fetalis, agenesis of corpus callosum, and cerebellar hypoplasia at the 26th week of gestation (Fig. 3). She was counseled that aneuploidy was suspected and offered genetic amniocentesis at the 25th week of gestation. Three weeks later the results of cytogenetic analysis of cultured amniotic cells revealed trisomy 9, a karyotype of 47, XY, +9 in all 64 of metaphase cells examined (Fig. 4). They were counseled regarding the poor prognosis of trisomy 9 and chose no further intervention for fetal indications at our hospital and only supportive care for neonate at the hospital near their residence. At the 32nd week of gestation, intrauterine fetal death was confirmed and on the next day, a stillborn male infant was delivered with a body weight of 875 g and a length of 39 cm after induction of labor. Macroscopic findings included small palpebral fissures, hypertelorism, micrognathia, low-set ears, hypoplastic phalanges, cryptorchidism, hypoplastic scrotum, micropenis, and rocker-bottom feet. Autopsy was declined by the parents.
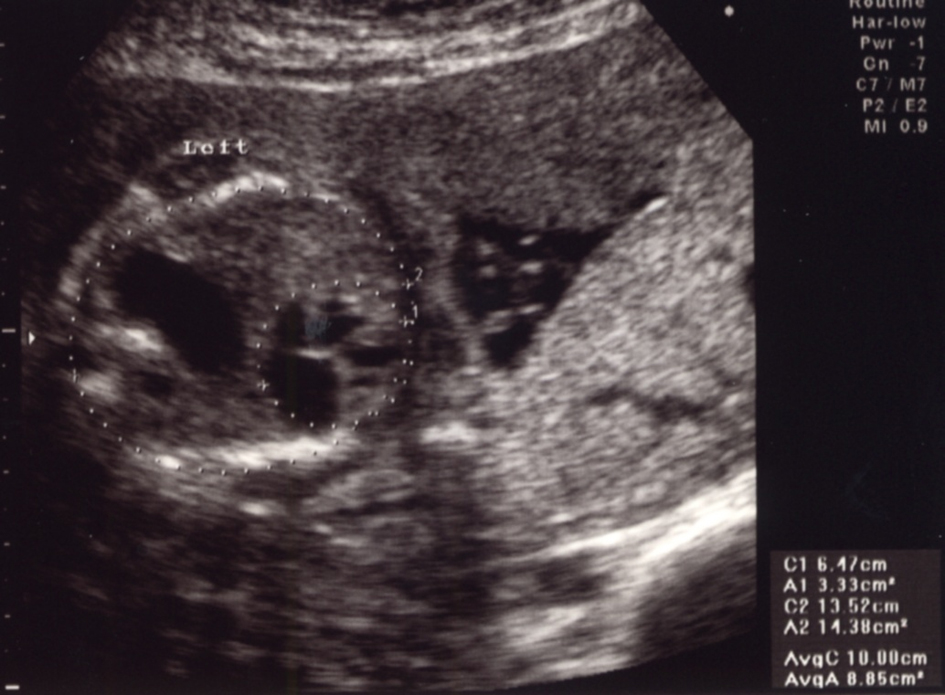 Click for large image | Figure 1. Prenatal ultrasound findings in a fetal thorax at the 25th week of gestation. Horizontal view of the thorax demonstrates a left-side diaphragmatic hernia and mediastinal shift. |
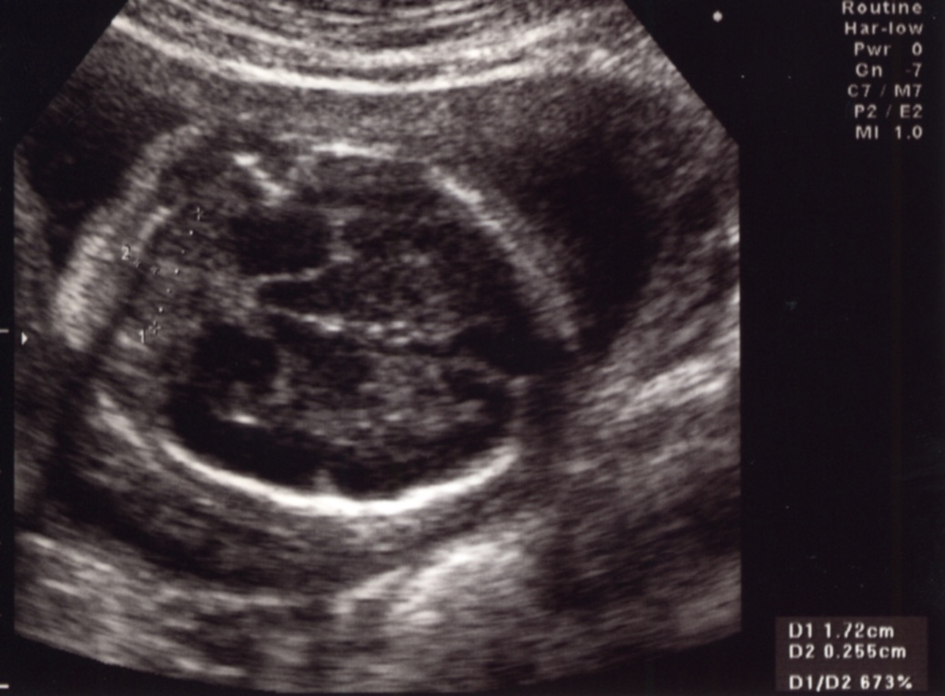 Click for large image | Figure 2. Prenatal ultrasound findings in a fetal head at the 25th week of gestation. There is ventriculomegaly and narrowing of cysterna magna. |
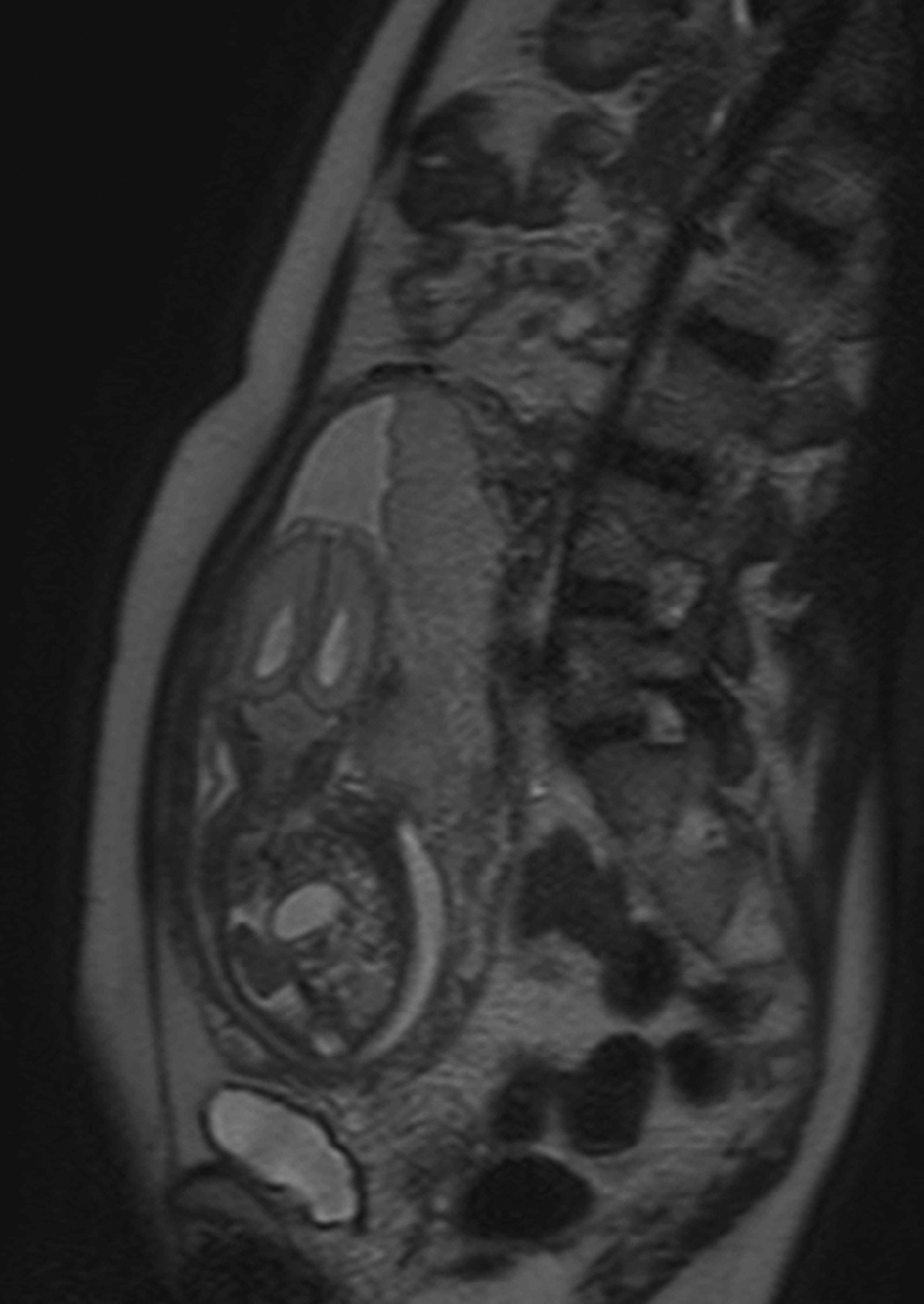 Click for large image | Figure 3. Prenatal MRI findings at the 26th week of gestation. CDH, hypoplastic left lung, agenesis of corpus callosum and cerebellar hypoplasia were revealed. |
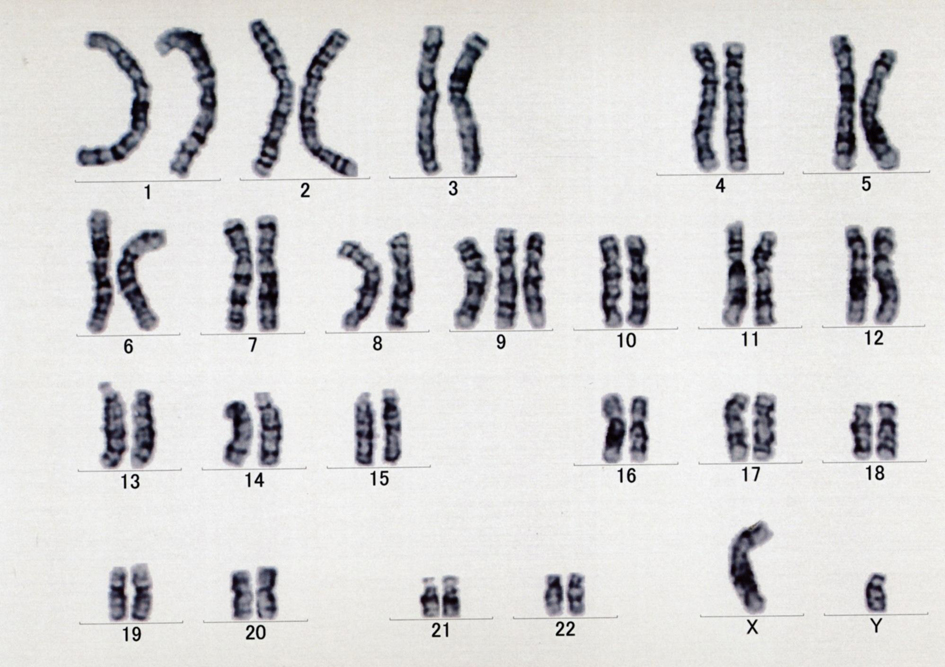 Click for large image | Figure 4. Karyotype at the 25th week of gestation. It shows 47, XY, +9. |
| Discussions | ▴Top |
Approximately from 60 to 90 % of CDH cases are detected prenatally either by ultrasound examination or by fetal MRI scan [6], so that fetal diagnosis could be easy. In this case, CDH was easily diagnosed because mediastinal shift and intrathoracic herniation of the bowel were noted in the 24th week of gestation by the ultrasound. CDH is also known to be associated with other malformations, and at least one associated malformation was diagnosed in about 36% of CDH [7]. In this case, ventriculomegaly and narrowing of cysterna magna were also observed by ultrasound. In addition agenesis of corpus callosum and cerebellar hypoplasia were diagnosed by MRI.
Chromosomal anomalies were presented in 9.5%, and the association of CDH with chromosomal anomalies such as trisomy 13 and 18 is well known [2]. In this case, karyotyping was performed to detect chromosome aberration and trisomy 9 was revealed. Trisomy 9 is a very rare chromosomal abnormality, occurring only 2.7% of all trisomic cases, so that most such cases result in first trimester spontaneous abortions and are rarely seen at near term [8]. Trisomy 9 has striking features in ultrasound findings including abnormalities of craniofacial, cardiac, skeletal, and genitourinary [9]. Prenatal diagnosis of trisomy 9 is difficult due to similarities to trisomies 13 and 18 in sonographic appearance [10]. In this case, we could not detect above anomalies in ultrasound findings but facial (such as small palpebral fissures, hypertelorism, micrognathia and low-set ears) and genitourinary (such as cryptorchidism, hypoplastic scrotum and micropenis) anomalies were detected by macroscopic findings after birth.
Prognosis of trisomy 9 is extremely poor and universally lethal [7] as well as trisomies 13 and 18. Most trisomy 9 fetuses are spontaneously lost, and prognosis of newborn infants with trisomy 9 is extremely poor. It was reported that 12 of 15 infants died within 1 month and one died within hours or days [11]. In this case, we could inform them about the poor prognosis of trisomy 9 because of accurate prenatal diagnosis by chromosomal analysis. They didn’t hope further intervention for fetal indications. After all, the fetus spontaneously died at the 32nd week of gestation. To the best of our knowledge, no cases of trisomy 9 with CDH have been reported in the English literature in Japan.
| References | ▴Top |
- Feingold M, Atkins L. A case of trisomy 9. J Med Genet. 1973;10(2):184-187.
doi - Witters I, Legius E, Moerman P, Deprest J, Van Schoubroeck D, Timmerman D, Van Assche FA, et al. Associated malformations and chromosomal anomalies in 42 cases of prenatally diagnosed diaphragmatic hernia. Am J Med Genet. 2001;103(4):278-282.
doi pubmed - Frohlich GS. Delineation of trisomy 9. J Med Genet. 1982;19(4):316-317.
doi pubmed - Sepulveda W, Wimalasundera RC, Taylor MJ, Blunt S, Be C, De La Fuente S. Prenatal ultrasound findings in complete trisomy 9. Ultrasound Obstet Gynecol. 2003;22(5):479-483.
doi pubmed - Chen CP, Chern SR, Cheng SJ, Chang TY, Yeh LF, Lee CC, Pan CW, et al. Second-trimester diagnosis of complete trisomy 9 associated with abnormal maternal serum screen results, open sacral spina bifida and congenital diaphragmatic hernia, and review of the literature. Prenat Diagn. 2004;24(6):455-462.
doi pubmed - Pober BR. Genetic aspects of human congenital diaphragmatic hernia. Clin Genet. 2008;74(1):1-15.
doi pubmed - Zaiss I, Kehl S, Link K, Neff W, Schaible T, Sutterlin M, Siemer J. Associated malformations in congenital diaphragmatic hernia. Am J Perinatol. 2011;28(3):211-218.
doi pubmed - Roshanfekr D, Dahl-Lyons C, Pressman E, Ural S, Blakemore K. Complete trisomy 9 in a term fetus: a case report. J Matern Fetal Med. 1998;7(5):247-249.
doi - Nakagawa M, Hashimoto K, Ohira H, Hamanaka T, Ozaki M, Suehara N. Prenatal diagnosis of trisomy 9. Fetal Diagn Ther. 2006;21(1):68-71.
doi pubmed - Yeo L, Waldron R, Lashley S, Day-Salvatore D, Vintzileos AM. Prenatal sonographic findings associated with nonmosaic trisomy 9 and literature review. J Ultrasound Med. 2003;22(4):425-430.
pubmed - Arnold GL, Kirby RS, Stern TP, Sawyer JR. Trisomy 9: review and report of two new cases. Am J Med Genet. 1995;56(3):252-257.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.








